Abstract
Background:
Spontaneous primary intracranial hemorrhage or known as intracerebral hypertensive hemorrhage consist of 15 to 20% of all stroke, is one of the major health problems among healthy and productive workforce in any countries.
Methods:
A retrospective study was conducted in a dedicated Neurosurgical Centre at the Hospital Sungai Buloh, Malaysia. The study was conducted for admission within a year period, in the year 2013 with 6 months follow-up. A total of 35 patients were studied.
Results:
The mean age was 52.8 years old (31-77 years old). A total of 29 patients (82.9%) were presented with basal ganglia hemorrhage, 4 with cerebral lobar hemorrhage (11.4%) and 2 with cerebellar hemorrhage (5.7%). The surgical mortality rate was 40%. For the 6 months follow-up, 31.4% patients improved to Glasgow Outcome score (GOS) of 4, while 22.9% and 5.7% patients improved to only GOS of 3 and 2 respectively. There were several factors identified in the study to be important predictors of survival. There were statistically significance of higher mortality rate among patients with pre-operative GCS of 5 and below (p=0.015), pre-operative CT scan brain showing acute hydrocephalus (p=0.046) and residual post-operative hematoma above 5% of pre-operative clots volume (p=0.006). Other factors such as age, sex, size of pre-operative hematomas, presence of intraventricular hemorrhage, underlying medical illness were not statistically significant in predicting the surgical outcome of those patients.
Conclusions:
Outcome predictors such as pre-operative GCS and CT scan brain findings helps treating neurosurgeons to determine the prognosis of patients presented with spontaneous intracranial hemorrhage.
Author Contributions
Academic Editor: Suraj Konnath George, MD Anderson Cancer Center
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2016 Liew Boon Seng, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Primary intracranial hemorrhage is one of the major health problems among productive workforce globally. It consists of 15 to 20 percent of all hypertensive strokes.1 Patients who suffer from hemorrhagic stroke tend to deteriorate faster than those who suffer from ischemic stroke.
There is a very small window of time or golden hour for the initiation of acute medical and surgical managements in this group of patients to achieve better outcomes. Surgical treatment for spontaneous intracranial hemorrhage includes craniotomy and evacuation of blood clots or it may also be just limited to implantation of an external ventricular drainage (EVD) without touching the hematoma. In the paper that all the patients underwent an operation to directly remove the clot which causing mass effect. Those patients with fast deteriorating conscious level, sizeable intracranial hematoma and fit to be subjected for a major cranial surgery under general anaesthesia are usually candidates for such procedures, mainly for life-saving purposes.2
A very small group of patients undergo such procedures due to potential of reversal the motor deficits caused by the hematomas. Surgical management may reduce early mortality in patient with large spontaneous superficial hemorrhage.3 Surgery also seems to reduce morbidity and dependency.4 Minimal invasive surgery may be beneficial in some studies.5
The objective of this paper is to determine the surgical outcome (mortality and morbidity) of patients with spontaneous primary intracranial haemorrhage underwent craniotomy and evacuation of clots. The secondary objective of the study is to identify predictors of survivals.
Materials and Methods
This is a retrospective cohort study conducted at Hospital Sungai Buloh, Malaysia. This study was conducted for admission within a year period with 6 months follow-up. A total of 35 patients who fulfilled the inclusion and exclusion criteria were studied. The selection of study subjects was based on the operation theatre registry. All selected patients were either admitted from the emergency department or referred from other hospitals. Those patients who computed tomography of brain showed a large hematoma and then were operated when the consultant Neurosurgeon considered it helpful (either directly after the arrival to emergency department, in other cases delayed if referred from other hospitals). The study was limited to only adult patients (18 years old and above) and all patients who underwent craniotomy and evacuation of clots irrespective of their pre-operative GCS (e.g. GCS of 3 was also included) or the time interval between decision of surgery and the actual surgery performed. Those patients who were diagnosed as secondary intracranial hemorrhage due to vascular, oncologic or hematological disorders were excluded. Inclusion criteria:
• All patients admitted between 1st January 2013 and 31st December 2013 who were diagnosed with spontaneous primary intracranial hemorrhage and underwent surgical evacuation of clot.
Exclusion Criteria:
• Further workup revealed secondary cause such as vascular malformation, aneurysm, tumoural bleed or hematological disorder.
• Patients who were transferred out to other centre post-operatively.
The null hypothesis for this study was that surgical evacuation of spontaneous primary hemorrhages does not improve the patient outcome.
Outcome at 6 months were evaluated using Glasgow Outcome Scale (GOS). The GOS was assessed directly by a Neurosurgeon during a clinical evaluation of the patient. IBM SPSS Statistics for Windows, Version 19.0 was used for statistical analysis. For categorical dichotomous variables, chi-square test was used but if any expected counts are less than 5 in more than 20% of the cells, Fisher’s exact text was used. The significant value was set at p value less than 0.05. Odds ratio (OR) and 95% confidence intervals (CI) were calculated.
Results
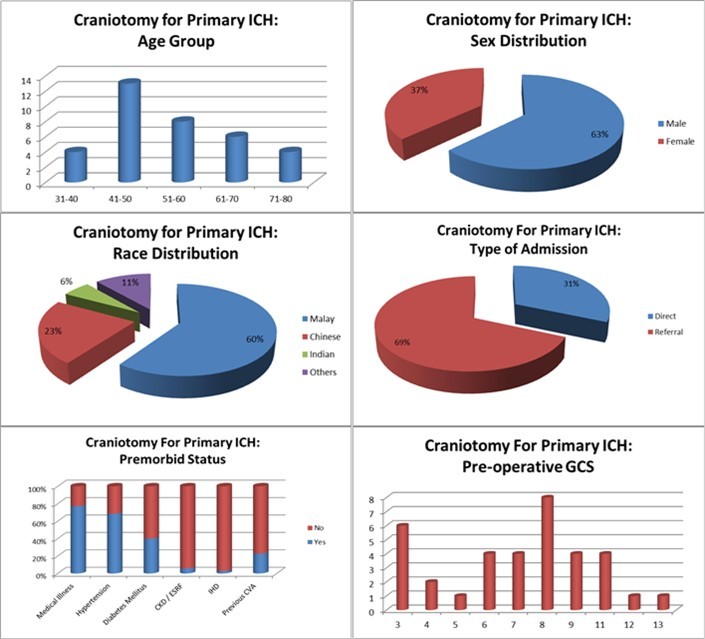
A total of 22 patients (62.9%) were from referring hospital and remaining 13 patients (37.1%) were direct admission. The mean age was 52.8 years old (range: 31-77 years old). About two-third of patients were male. Most patients were Malays, followed by Chinese and other races. About one-third patients were admitted directly while another two third were referred from other institutions. 77.1% patients were with history of premorbid illnesses. Most patients suffered from hypertension followed by diabetes mellitus, history of previous cerebrovascular accident, renal impairment and ischemic heart disease. (Figure 1)
CKD= Chronic kidney disease; ESRF=End-stage renal failure; IHD=Ischemic heart disease; CVA=cerebrovascular accident
Most cases involved the right cerebral hemisphere. Twenty nine patients were presented with basal ganglia hemorrhage, four with cerebral lobar hemorrhage and two with cerebellar hemorrhage. 71.4% patients were presented with admission GCS of 8 and below. In most patients, the volume of the hematoma was between 30 and 49 ml. Only two patients with volume of hematoma exceeding 90 ml. 60% patients presented with intraventricular hemorrhage and 37.1% patients with obstructive hydrocephalus. (Figure 2)
Figure 2.ICH – Anatomical location, volume and its complications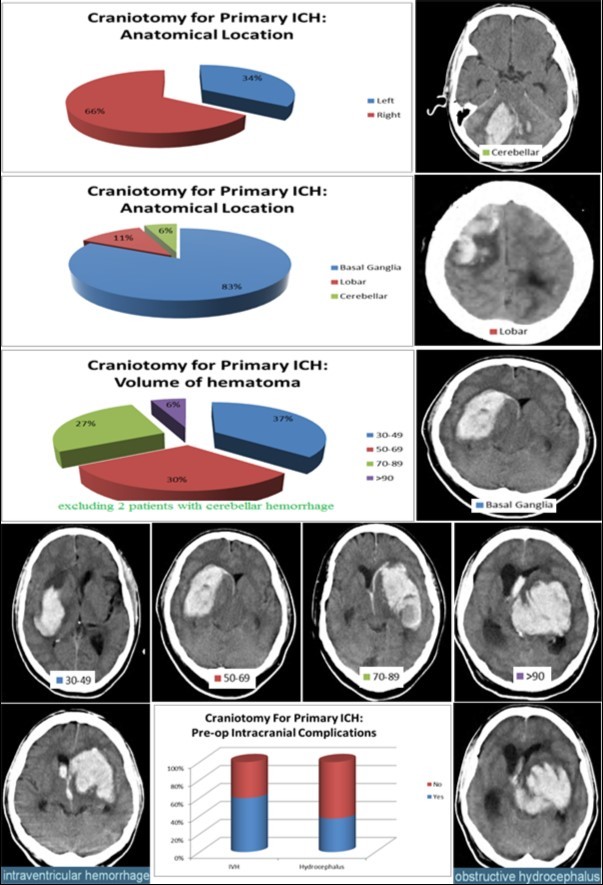
There was inverse correlation between admission MAP and volume of pre-operative hematoma, with the exception of hematomas larger than 90 ml, associated to higher blood pressure. (Figure 3)
Figure 3.Relationship between pre-operative ICH volume and MAP and the effect of post-surgical evacuation of hematoma on SBP and DBP
The surgical mortality rate was 40 percent. All fourteen deaths reported in this study were during initial admission. Seven deaths (20.0%) were due to intracranial hemorrhage without complication from other organ failure. Other deaths were complicated with acute kidney injuries (four patients, 11.4%), septicemia (two patients, 5.7%) and non-ST elevation myocardial infarction (one patient, 2.9%). For surviving patients at 6 months follow-up, eleven (31.4%) patients improved to a favourable state, while ten (28.6%) patients remained at unfavourable state. Mean GOS was lowest at 1.67 among patients with admission GCS of 3 to 5 and highest at 4 among patients with admission GCS above 11. (Figure 4)
Figure 4.Glasgow Outcome Scale at 6 months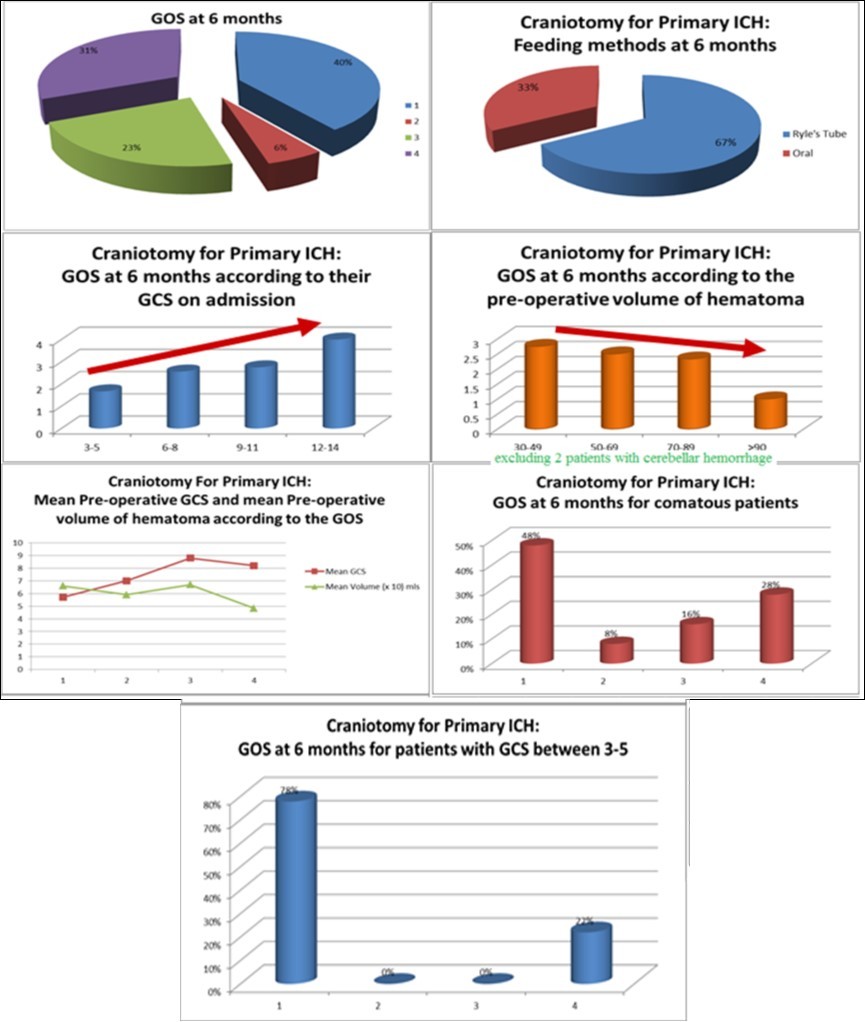
There were several factors identified in the study to be important predictors of non-survival. There were statistically significant of higher mortality rate among patients with pre-operative Glasgow Coma Scale (GCS) of 5 and below (OR for death = 9.5; p=0.015) and pre-operative CT scan brain showing acute hydrocephalus (OR for death = 4.3; p=0.046). All patients with post-operative residual hematoma above 50% of pre-operative clots volume due to rebleeding died after the surgery (p=0.006). (Table 1) Other factors such as age, size of pre-operative hematomas, intraventricular hemorrhage and underlying medical illness were not statistically significant in predicting the surgical outcome in those patients.
Table 1. Factors associated with rate of survival at 6 months follow-up| Survived n (%) | Death n (%) | OR (95% CI) | P Value | |
| Pre-operativeGCS GCS < 5 GCS >5 | 2 (22.2) | 7 (77.8) | 9.5 (1.58-57.2) | 0.015f |
| 19 (73.0) | 6 (22.2) | |||
| Hydrocephalus | ||||
| Yes | 5 (38.5) | 8 (61.5) | 4.3 (1.0-18.4) | 0.046p |
| No | 16 (72.7) | 6 (27.3) | ||
| Residual hematoma | ||||
| < 50% | 0 (0.0) | 5 (100.0) | - | 0.006f |
| >50% | 21 (70.0) | 9 (30.0) |
Discussion
Surgical evacuation of spontaneous intracerebral hematomas is basically required to control intracranial pressure. Especially in younger patients with uncontrolled blood pressure, large clots and evolving neurological impairment the surgical treatment represents the final and main step for life saving. In reality, due to high surgical mortality and morbidity, the first treatment option for spontaneous primary intracranial haemorrhage is always medical therapy, especially in patients with intact conscious level. However, in those patients with deteriorating conscious level or those with evidences suggesting of raised intracranial pressure, refractory to medical therapy, surgical treatment is always offered as the last treatment option available. Due to current practices, patients treated with both surgical and medical treatments usually have worse outcome than those with medical therapy alone. However, there were also many publications which suggest that mortality rate may be reduced with combination of surgical and medical treatments than medical therapy alone.2,7,8 (Figure 5)
Figure 5.Comparison of state of consciousness at presentation and 6 months mortality in patients with Primary ICH subjected for either medical or surgical treatments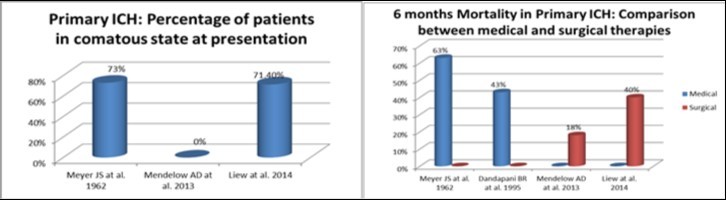
The most important consideration to be made is whether the clinical status of the referred patient is considered at the level which considered as indicated for surgery. Current guidelines do not give clear selection criteria for patients who will be benefited from cranial surgery due to spontaneous primary intracranial haemorrhage. In this paper, the overall surgical outcome was considered poor, with mortality rate of 40%. However, above 70% of patients were in comatose state pre-operatively. In non-comatose patients, the outcome in this study was comparable to STICH II study.2 (Table 2)
Table 2. Characteristic of non-comatose patients with primary ICH and their surgical outcome in 2 different studies| Non-comatose patients | Mortality (%) | Good Outcome (%) | Mean GCS | Mean volume (ml) |
| Mendelow AD et al. 2013 | 18 | 36 | 12.9 | 41.4 |
| Liew et al. 2014* | 20 | 40 | 10.5 | 50.9 |
| Lobar: 1 patient (10.0%) | ||||
| Basal ganglia: 9 patients (90.0%) |
There are also no clear guidelines available on the cut off age for surgical candidate. In this study, the eldest patient was at 77 years old. Generally, surgeon is guided by the volume of hematoma to decide on the surgical option. However, interestingly, those patients presented with smaller volume of intracranial hematoma presented with higher mean arterial pressure, while those patients with larger volume of intracranial hematoma presented with lower mean arterial pressure, with exceptional of those with volume of intracranial hematoma beyond 90 ml. Higher mean arterial pressure with deteriorating conscious level may also indicating raised intracranial pressure, especially in those with bradycardia. CT evidences of raised intracranial pressure includes effaced basal cistern, sulci and gyri not well visualised, slit-like ventricles and midline shift. This findings may suggest surgical treatment may not only decided based on the volume of intracranial hematoma but also other clinical parameters and CT scan findings such as midline shift and effacement of basal cistern. Optimization of BP in both SBP and DBP were achieved post-operatively following removal of intracranial mass lesion.
All patients were only subjected to single procedure of craniotomy. None of patients in the study including those with residual blood clots above 50% of initial clot size were subjected for repeat surgery. However additional procedures such as external ventricular drainage were performed in patients with intraventricular hemorrhage and hydrocephalus and tracheostomy were performed in those with poor recovery of conscious level.
There was positive correlation between Glasgow Coma Scale on admission and the GOS at 6 months. In terms of Glasgow Coma Scale, this study shows that patients with pre-operative Glasgow Coma Scale 5 and below have significantly higher risk of death after surgical treatment.(OR for death = 9.5, p=0.015) There was negative correlation between pre-operative volume of hematoma and mean GOS at 6 months. There were only two patients (6%) were on pre-treatment of aspirin. They underwent platelet transfusion prior to surgery. Both were presented with clot volume of above 60 ml. However only one of them with post-operative residual blood clot volume above 50% and survived, while the other one were with post-operative blood clot volume below 50% and died from the intracranial cause. The association between the expansions of hematoma with premorbid use of antithrombotic drugs cannot be proven conclusively with current published literatures. Both patients with size of hematoma exceeding 90 ml did not survive after the surgery. Despite association between size of pre-operative hematomas and outcome was not proven statistically, patients with lower GCS on admission and larger size of hematoma had poorer outcome at 6 months compared to patients with better GCS on admission and smaller size of hematoma. Patients with GCS of 5 and below on arrival were the poorest candidate for surgery.
Another important finding from this study is the volume of residual hematoma post-operatively. The post-operative volume of hematoma may be due to many factors such as poor hematoma evacuation, rebleeding due to poor blood pressure control post-operatively or may be due to deranged coagulation profile post-operatively. However, interestingly those patients with residual volume of hematoma above 50% did not survive. This important finding may suggest inadequate intracranial pressure control.
The association of patient’s age, volume of pre-operative hematoma, presence of intraventricular haemorrhage and pre-morbid status with the surgical outcome were not proven statistically in this study. These important findings may show that the age may not be the limiting factor for surgery. The importance of clinical worsening especially among younger patients who were not comatose at admission should be prioritized by the neurosurgeons in their surgical decision-making. The presence of intraventricular haemorrhage and large volume of intracranial hematoma are not associated with poorer outcome. So those patients with these two findings may not be ruled out as surgical candidate if their clinical status allows safe surgical treatment. Although intraventricular haemorrhage may not be associated with poorer outcome, this study shows pre-operative CT showing acute hydrocephalus is a significant predictor of mortality. (OR for death = 4.3, p=0.046)
There is no evidence to demonstrate any form medical therapy such as corticosteroids, glycerol or mannitol that can successfully reduce mass effect of ICH.9, 10, 11Therefore, surgical treatment of selective patients with significant spontaneous primary intracranial haemorrhage may still be an important treatment modality. Early surgical management in those patients may allow better surgical outcomes. Patients with very poor Glasgow coma scale may be treated with medical therapy alone.
Conclusion
In this study, majority of patients who have undergone craniotomies were those with basal ganglia hemorrhage. Hence, we can conclude that surgical evacuation of hematomas in selected patients with basal ganglia hemorhage may be beneficial. However due to high percentage of surgical mortality, the need of surgical management should be discussed and decided as a case-by case basis. Pre-operative GCS and the presence of hydrocephalus in CT scan brain are important predictors which can be used by treating doctors to discuss with the patients' family regarding their prognosis. Those with presenting GCS of 5 and below and large pre-operative hematomas should not be subjected to surgery.
Limitations
It is a retrospective 35 patients cohort, with 29 basal ganglia, 4 lobar hemorrhages and 2 cerebellar hemorrhages and several selection biases. There was lack of information of those patients receiving medical therapy alone at the referring hospitals. Hence those receiving medical therapy alone could not be analyzed for comparison. A multi-centers study is needed in the future study to avoid bias in the analysis of the outcome which dependent on the center-specific technique-related effect and to allow direct comparison between surgical and non-surgical management of spontaneous primary intracranial hemorrhage.
References
- 1.Dennis M S, Burn J P, al Sandercock PA at. (1993) Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. , Stroke 24, 796-800.
- 2.Mendelow A D, Gregson B A, Rowan E N.(Aug3,2013) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial.Erratum in:Lancet.2013Aug3.382(9890): 396.Epub2013May29.Lancet. 382(9890), 397-408.
- 3.R Samprón N, Mendia A, Azkarate B.(Apr2010) Early mortality in spontaneous supratentorial intracerebral haemorrhage. , Neurocirugia (Astur) 21(2), 93-8.
- 4.Prasad K, Shrivastava A. (2000) Surgery for primary supratentorial intracerebral haemorrhage. Cochrane Database Syst Rev.(2):CD000200.Review.
- 5.Zhou X, Chen J, Li Q.(Nov2012) Minimally invasive surgery for spontaneous supratentorial intracerebral hemorrhage: a meta-analysis of randomized controlled trials. , Stroke.Epub2012Sep18 43(11), 2923-30.
- 6.Jennett B, Bond M.(Mar1,1975) Assessment of outcome after severe brain damage. , Lancet 1(7905), 480-4.
- 7.Meyer J S, Bauer R B. (1962) Medical treatment of spontaneous intracranial hemorrhage by use of hypotensive drugs. , Neurology 12, 36-47.
- 8.Dandapani B R, Suzuki S, Kelly R E. (1995) Relation between blood pressure and outcome in intracerebral hemorrhage. , Stroke 26, 21-24.
- 9.Poungvarin N, Bhoopat W, Viriyavejakul A. (1987) Effects of dexamethasone in primary supratentorial intracerebral hemorrhage. , N Engl J Med 316, 1229-1233.