Abstract
Objective:
Demographic analysis of intrauterine deaths in North-Eastern Hungary with national and international comparison.
Materials and Methods:
The authors collected data from the National Bureau of Statistics’ 1996-2014 database to assess frequency, gestational age, maternal age and education for six counties of the region. 722 individual cases were analyzed. A regional survey was initiated to collect more detailed data on living environment in the region between 2010 and 2014 through community midwifery services records.
Results:
Data over 20 years showed most intrauterine deaths (Perinatal mortality, Late fetal death, Stillbirth] occurred between 24th and 36th weeks of which 35% occurred in the North-Eastern region of Hungary. The causes of intrauterine deaths were placental abruption, cord accident, placental insufficiency, malformations and intrauterine infection. Detailed analysis regarding attendance at either the Obstetricians or the community midwifery services, the patient’s medical history and the patients’ compliance were reported, compliance in 1% completely lacked. Gravidity and multiparity were associated risk factors. A significant proportion was associated with teenage pregnancy, low maternal education, smoking risks, unemployment, dependence on social support, unhygienic environment and smaller accommodations. Lack of cooperation during antenatal care was significant.
Conclusion:
Frequency and distribution of intrauterine deaths in North-Eastern Hungary show a similar picture as those of socio-economic indices. The unfavorable trend came to an end in 2015, however the national statistics did not show any improvement. The solution to the problem seems to be independent of the service provision, therefore, socio-economic development of affected counties is warranted, and financial incentives and/or government aid provided during pregnancy may improve future perinatal outcomes.
Author Contributions
Academic Editor: Ying-Chu Lin, Kaohsiung Medical University, Taiwan, Email: [email protected]
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Singh Jashanjeet, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Perinatal mortality consists of late fetal death (Stillbirth), and early infant death. Late fetal death implies fetal death prior to the complete expulsion/extraction from the mother of the product of human conception, upon completion of 24 gestational weeks, irrespective of the duration of pregnancy, which, after such expulsion/extraction shows no signs of life. Early infant death is death of an infant within one week of live birth. In Hungary, following the international recommendations live born fetus is one that was extracted/expulsed from the mother and shows any signs of life (respiratory or cardiac activity, umbilical cord pulsation) which is regardless of its womb age and survival 1. Between 1990-2011 within perinatal mortality there was an increase in late fetal death and decrease in early infant mortality ratio. The change was firstly, due to a switch from 28th to 24th gestational week in the international standard definition in 1996 that automatically increased the number of late fetal deaths and the ratio of all fetal deaths and secondly, the number of premature infant deaths occurring between 0 and 6 days, which played a role in the reduction of general infant mortality, fell more than the average. Thus, among the two components of perinatal death the first ones’ importance increased while the other shows continuous decrease. In 1990, perinatal death represented 39% of late fetal deaths and 61% early infant deaths. These rates turned around by 2011. The proportion of late fetal deaths rose to 67% while early infant death decreased to 33% 1. Recently, there is no significant improvement shown in the prematurity rate. Between 1990-2011 7%-9% of children were born prematurely and perinatal mortality fell from 14% to 7%. The decrease is significant in case of 0-6-day mortality, which shows 76% improvement attributable to obstetric care improvement, but especially due to development of neonatology and neonatal intensive care units 1.
In 2014, the World Health Assembly, which decides policies for the World Health Organization agreed to a target of 12 or fewer stillbirths per 1000 births in every country by 2030 (International Stillbirth Alliance), which has not been approached yet. World Health Organization in 2016 reported Stillbirth: A neglected tragedy, where it highlighted that 98% of deaths occurred in low and middle income countries 2. Low socioeconomic status is a risk factor for preterm delivery, low birth weight and stillbirth as well. Therefore, requiring attention to the fact that financial shortcomings may alter the outcome thus, making it a preventable risk factor. A study among the Roma and non-Roma communities highlighted the fact that poor socio-economic and behavioral characteristics correlated with poor birth outcomes 3. Along with lower socio-economic conditions domestic violence increased the likelihood of single or repeated fetal loss 4, 5, 6.
Between 2010-2014 in the North-eastern region of Hungary the number of intrauterine deaths slightly but continuously increased 7. This lead us to answer the following questions.
Is it all about trends?
What is the situation in the region and worldwide?
Any identifiable causes?
Can the profession contribute?
Materials and Methods
In the north-eastern twin region of Hungary, we analyzed data regarding intrauterine deaths, the developments and the most important components regarding perinatal mortality to identify the influencing causes. The Central Statistical Office (KSH) collected data from the six counties in the north-eastern Hungary for cases from 1996 to 2014 (Nógrád, Heves, Borsod-Abaúj-Zemplén (BAZ), Jász-Nagykun-Szolnok (JNSz), Hajdú-Bihar (HB) and Szabolcs-Szatmár-Bereg (SzSzB) counties the annual number of late fetal deaths, in each case, the respective gestational age, maternal educational level and maternal age 1, 8, 9, 10. For a more detailed analysis of the rising number of cases between 2010 and 2014, the background collecting data, we utilized the services of the six-counties district midwifery services. The perinatal deaths over the decades were analyzed in detail in the annual regional meetings regarding prenatal care, obstetric and neonatal professionals involved in care. Although in the recent years due to reorganization, the regular audit of this form disappeared, however, the nurses' data collection continued in most counties. In Heves county, for example, each case of 150-point questionnaire recorded the data on obstetric, medical, healthcare in addition to housing, social and economic conditions of the whole family. Data collection included the identified cause of death in the womb, a gestational age, fetal gender, birth weight, place and method of delivery, parity, gravidity, the medical history, diseases during pregnancy, visit to obstetric care facilities, consultations with mid wife/community nurse, completion of screening tests, willingness to cooperate with mid-wife/community nurse and doctor, the mother's level of education and her occupation, access to social benefits, unemployment incidence in the respective families, housing with degree of comfort and hygienic conditions, the number of rooms and the number of co-residents, personal and family use of tobacco and alcohol, psychological state during pregnancy, anxiety, the incidence of neurotic or psychotic signs, couples with strained relationships, certain elements of the supply system (family support services, child welfare services, specialist obstetrician, pediatrician, family physician, community nurse) availability at the place of residence. Given the data sheets were electronically recorded and suitably structured for processing nature, the other counties in the region following this data structure, also collected data. In some cases, we used the help of several hospitals in the region with the review of the medical data. The multi-parameter data analysis was performed by processing 722 cases. In the region, intrauterine death was compared to national and international data, in which we used the KSH and the Lancet Stillbirth in High Income Countries Working Group data 10, 11.
Results
In Hungary, the number of intrauterine deaths changed in the last 20 years (Figure 1) between 378 and 556 per year. Although, the trend shows an improvement in the long term, but there is concern that over the past few years, the number of cases have increased. In the year 2015, 434 pre-natal fetal deaths have been reported in the country in the in-patient care institutions. In the north-eastern twin region of Hungary between 2010 and 2014 the number of registered cases showed a rising frequency, however, in 2015 it has showed significant improvement. Across the region, the number of dead fetuses in 2015 was 126 in utero, which is equivalent to the 2010 levels. It is less gratifying that over the past 20 years, all the deaths that occurred in the country before giving birth, of these 35% of pregnant women were from the northeastern region. In this region 26.8% of the country’s population resides and 28.2% of births took place here. To be able to provide a more accurate assessment of the causes and social conditions is how our survey began, however, in the Jász-Nagykun-Szolnok county it was unsuccessful. Szabolcs-Szatmár-Bereg county, Nyíregyháza and Kisvárda Obstetric Departments helped us to make up for the missing data. Debrecen Department of Obstetrics and Gynecology and the Berettyóújfalu hospital staff helped us gathering valuable additional data 12.
Figure 1.Late fetal deaths in Hungary and Northeast Hungary between 1996 and 2014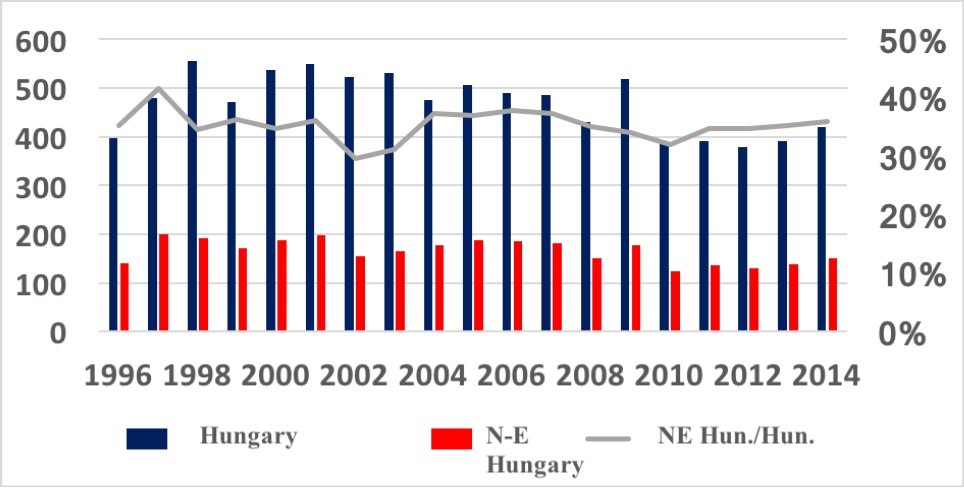
Figure 2.Late fetal deaths in the counties of the North-Eastern twin region between 1996 and 2014
Comparing the six counties of this region it can be concluded that unfavorable figures especially in the economic and social figures of the Borsod-Abaúj-Zemplén and Szabolcs-Szatmár-Bereg counties were most disadvantaged. Other possible explanations that were examined were the frequency of teenage pregnancies that complicated intrauterine events. According to the KSH data, in the last 20 years, the number of intrauterine deaths is consistently less than 10% in case of teenage pregnancies (Figure 3). In totality in these counties’ region the figure is not higher, but in Borsod-Abaúj-Zemplén county 20% of the cases and Szabolcs-Szatmár-Bereg county is close to 15% where pregnant women were under 20 years of age (Figure 4). The teen pregnancies frequency varies widely in the Northeastern region. In Borsod-Abaúj-Zemplén it is 10%, and in the Hajdú-Bihar county only 1% of pregnancies are in women less than 20 years of age. In comparison, of intrauterine deaths affected in intrauterine pregnancies Borsod-Abaúj-Zemplén County: 20% were affected, however in Hajdú-Bihar county it was practically 0% of teenage pregnancy rate. On this basis, we can confirm that intrauterine death may be linked to or is influenced by teen pregnancy as well.
Figure 3.All cases of late fetal deaths and cases of among 15-19 years old in Hungary between 1996 and 2014.
Figure 4.Late fetal deaths among 15 and 19 years old pregnant women in the counties between 1996 and 2014.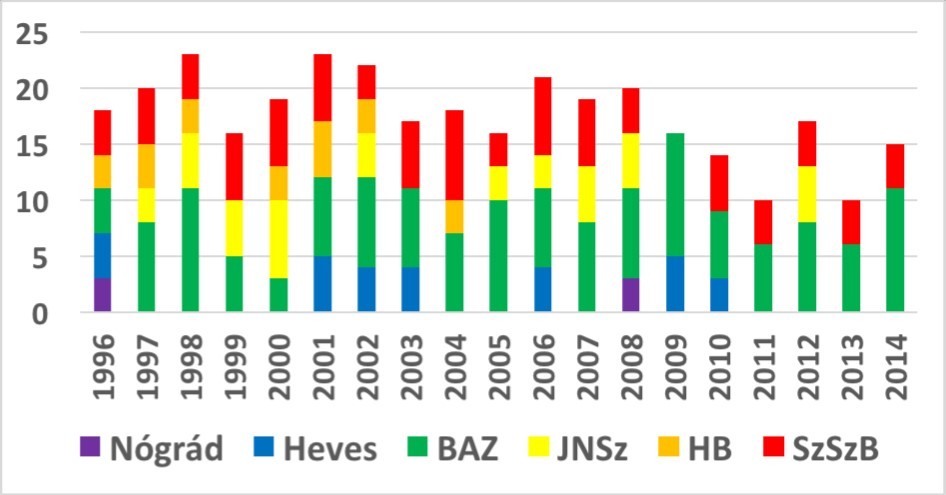
Over the past 20 years among intrauterine deaths approximately in 5% of the cases the mother’s level of education did not reach the 8th grade (Figure 5). In the Northeast region, this ratio exceeded 10%. In the period between 2010-2014 the region registered such cases in all 6 counties except for expecting mothers living in Borsod-Abaúj-Zemplén county (Figure 6).
Figure 5.All late fetal deaths and total number of patients who completed between 0-7 years of primary school education in Hungary between 1996 and 2014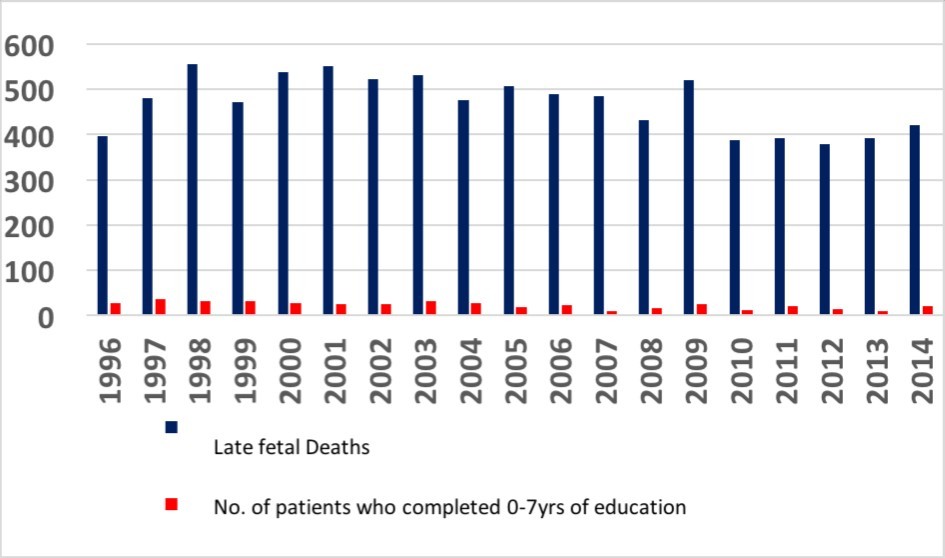
Figure 6.Late fetal deaths among patients in counties who completed between 0-7 years of primary school education in Hungary between 1996 and 2014.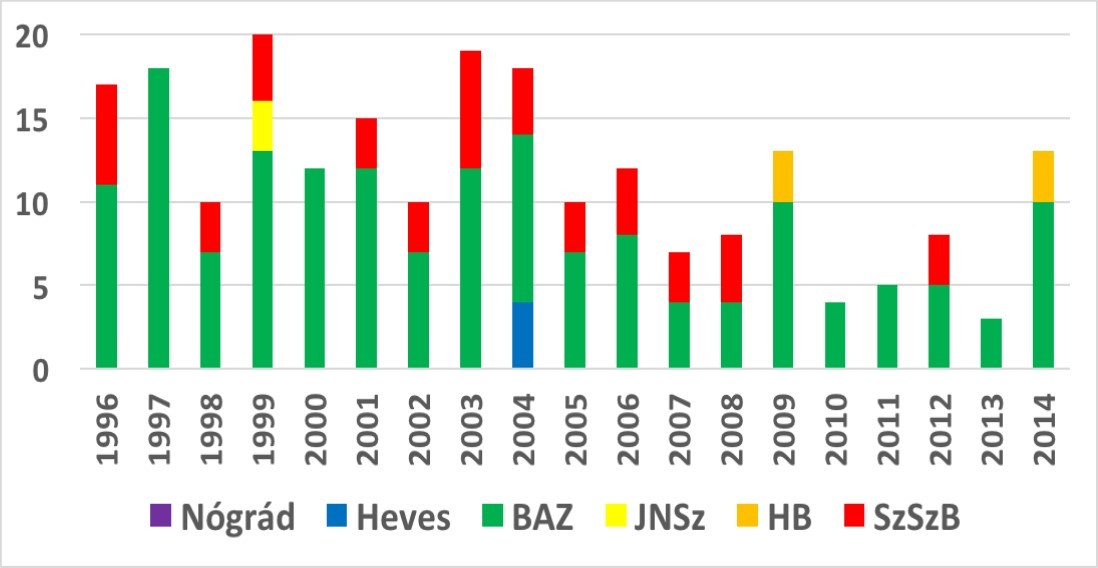
The distribution of gestational age, according to KSH data, between 1996-2014 in 2 / 3-3 / 4-scale the majority of the cases occurred in pregnancies between the 24th-36th weeks (Figure 7). In the region's counties, it is even more striking that except for a small proportion of cases, typically 80-90% of the cases involving intrauterine death occurred prior to the 37th week. (Figure 8).
Figure 7.Late fetal deaths at 0-23; 24-36; 37-x and unknown pregnancy weeks in Hungary between 1996 and 2014.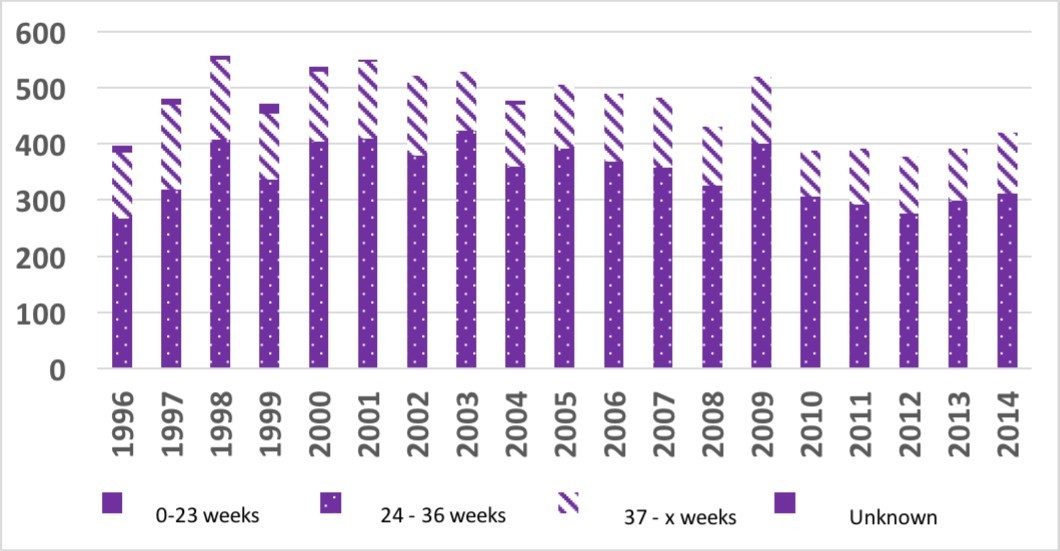
Figure 8.Late fetal deaths in the 0-23, 24-36, 37-x, and unknown pregnancy week in the northeastern twin region by county for the period between 1996-2014.
We investigated 722 cases in northeast Hungary to consider the causes and circumstances of intrauterine death. Among the identified causes in descending order of frequency were placental abruption (26%), umbilical cord complications (17%), placental insufficiency (14%), fetal malformation (4%) and intrauterine infection (2%) occurred in these cases (Figure 9). In 34% of the cases the causes of intrauterine death, reason could not be established. The sex ratio showed insignificant majority in favor of female fetuses (Figure 10). The clear majority of births took place in-patient obstetric care institutions, whereas only 22 of the 722 cases that took place outside these institutions. None of these were planned home births. 37% of intrauterine births were delivered by Caesarean section. The main reason for this may be due to the fact that a significant proportion of these pregnancies had maternal complications. The fetuses were below 1000 grams in 16.5% of cases and 22.4% were term. Like the gestational age distribution of our region it was proven that dead fetuses weighing less than 2500 grams was 77.6%.
Figure 9.Identified causes of intrauterine deaths.
Figure 10.(a) Gender of the dead fetus, (b) Mode of Delivery, (c) Birth place either as an in-patient or outside an inpatient facility either planned or unplanned, and (d) Birth Weight Distribution.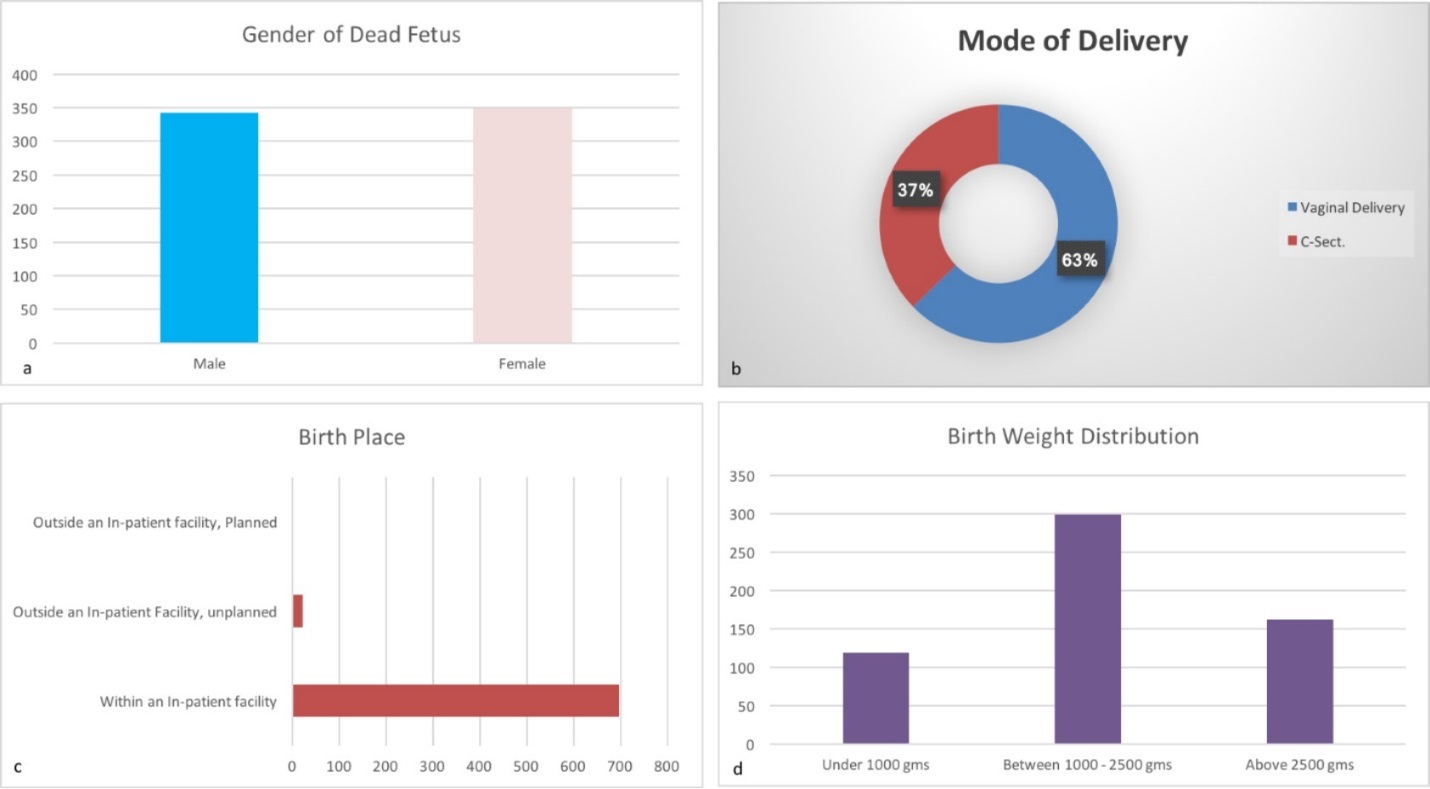
Most of the parents had more children (mean 2.5), the average number of pregnancies was 3.2 (Figure 11). Among the 722 cases out of which 139 (19%) had at least the fifth pregnancy, intrauterine death occurred in 84 (12%) had delivered more than four times before. 221 patients (31%) had sickness during pregnancy, 156 (22%), were justified to have increased health care surveillance. Despite this, 51 (7%) of cases the pregnant mother did not appear at the obstetric care facility, but was visited by the district nurse. Moreover in (1%) not even the nurse visit was recorded.
Figure 11.(a) Respective Parity and Gravidity, (b) Grand multigravidity and multiparity, (c) Patients who needed increased surveillance and (d) Patients who did not appear for counseling.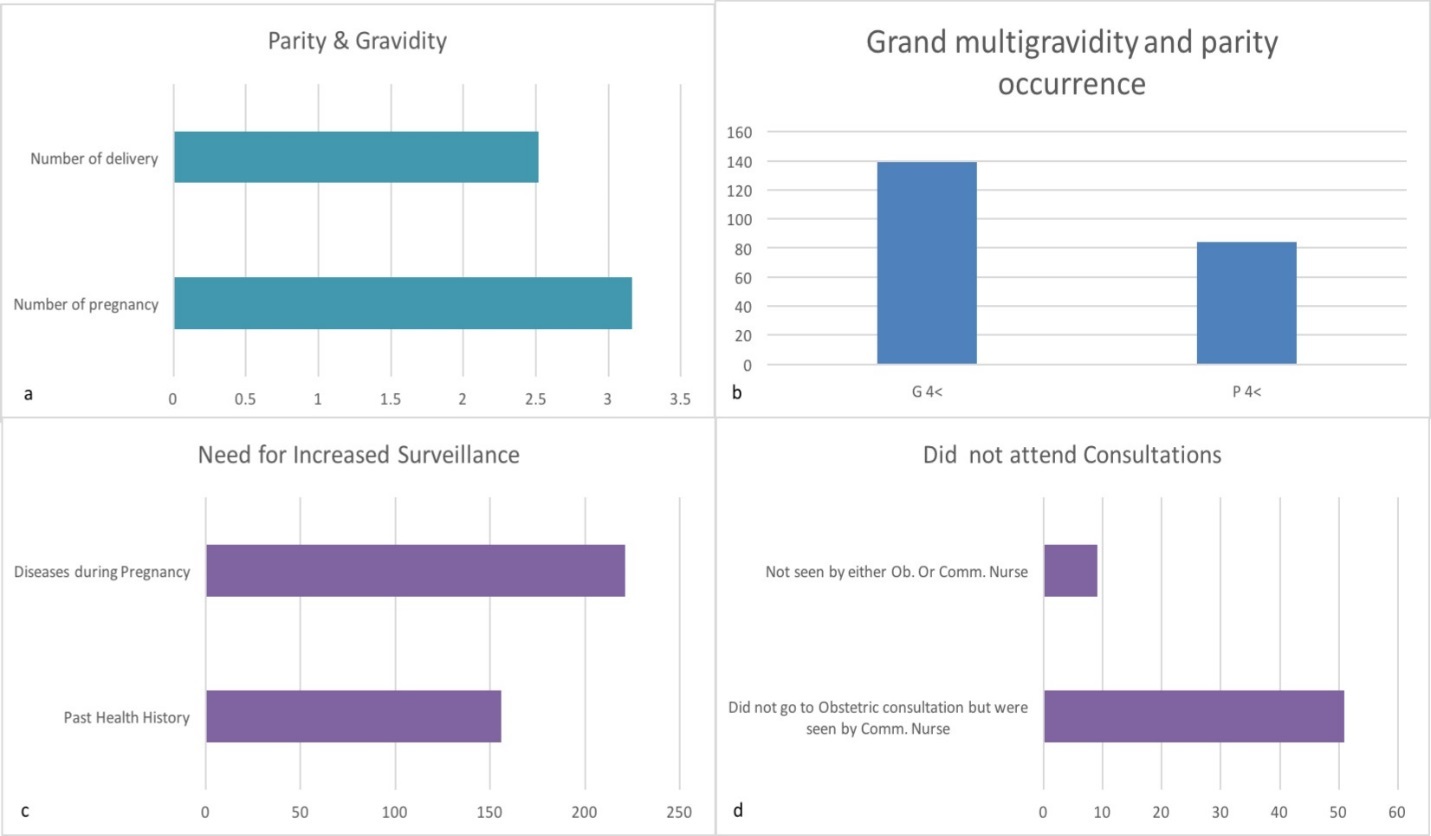
In half of the cases the mandatory screening tests were complete, but in 163(23%) cases they were not performed (Figure 12). In 43% of cases with the doctor and in 44% of cases with the community nurse/district mid-wife collaboration was missing. 22% of pregnant women had attended primary schools, 7% had not even attended 8 years of primary school education, either. The unemployment rate was 29%.
Figure 12.(a) Patients who completed screening tests, (b) Compliant cases (how they co-operated either with the Phhysician or Community Nurse, (c) Education level and (d) Maternal employment distribution.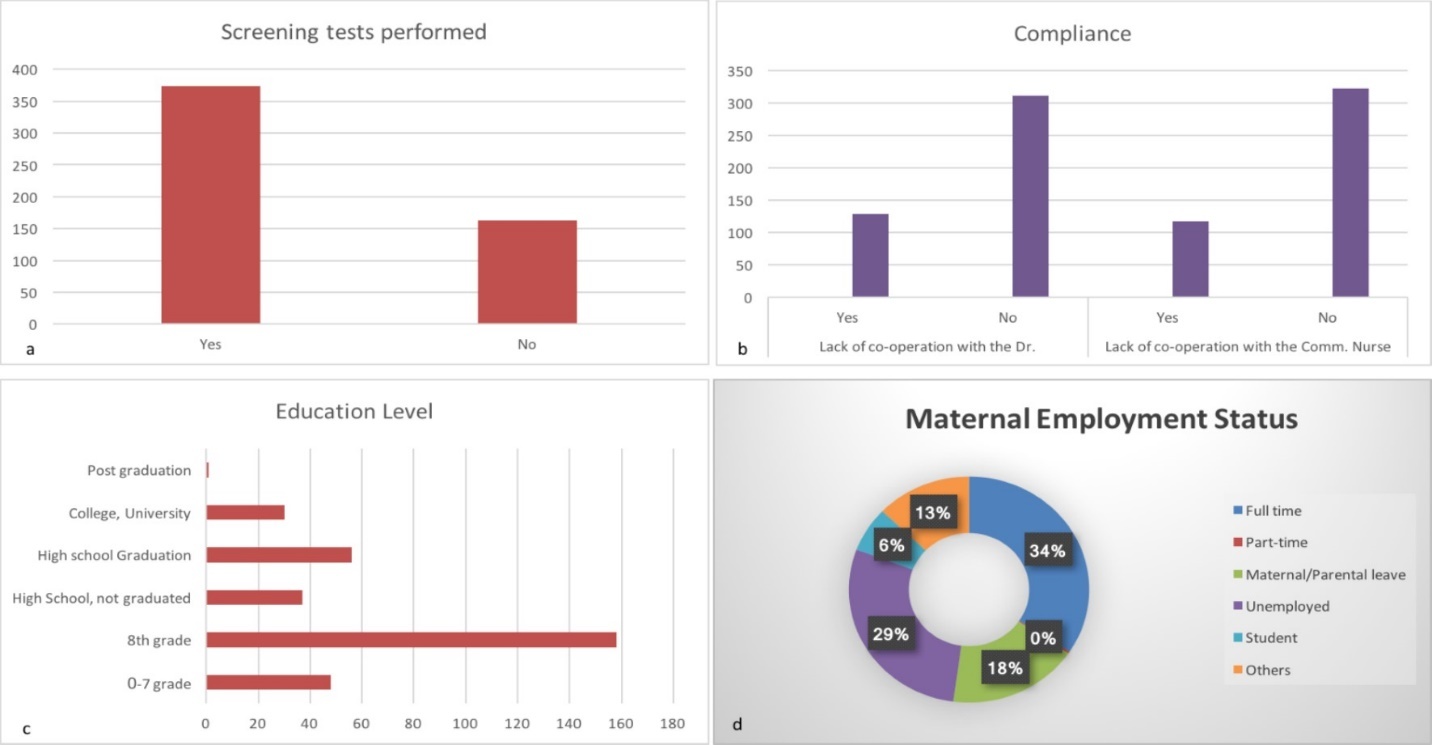
In 20% of pregnant women (147 cases) were receiving regular social assistance, 207 cases (29%) there was unemployment in the family (Figure 13). Among pregnant women, 37% (118 cases) lived without comfort, 30% of them had a one- or a two-bedroom apartment. In 15% of cases more than 5 persons lived in the same apartment. Regarding, inadequate or neglected residential sanitation incidence was 30%.
Figure 13.(a) Social status as to aid beneficiary or unemployment, (b) Patient Hygiene, (c) Living conditions-No. of people living together, (d) Number of rooms available in the patient’s house and (e) Patient’s standard of living.
Among the 722 cases, 227 where the mother, in 181 husband/partner, and in 136 cases people in the living environment smoked (Figure 14). Regular alcohol consumption was recorded for 12 pregnant women, 35 husband/partner and for both together in 26 cases. 47 pregnant women had anxiety, such as abnormal mental state but it was concluded that neurotic or psychotic symptoms did not occur. Relationship crisis was found for 47 pregnant women before mortality in utero.
Figure 14.Distribution of high risk behaviors: (a) Smoking, (b) Consumption of alcohol, (c) Psychological state and (d) Relationship problems.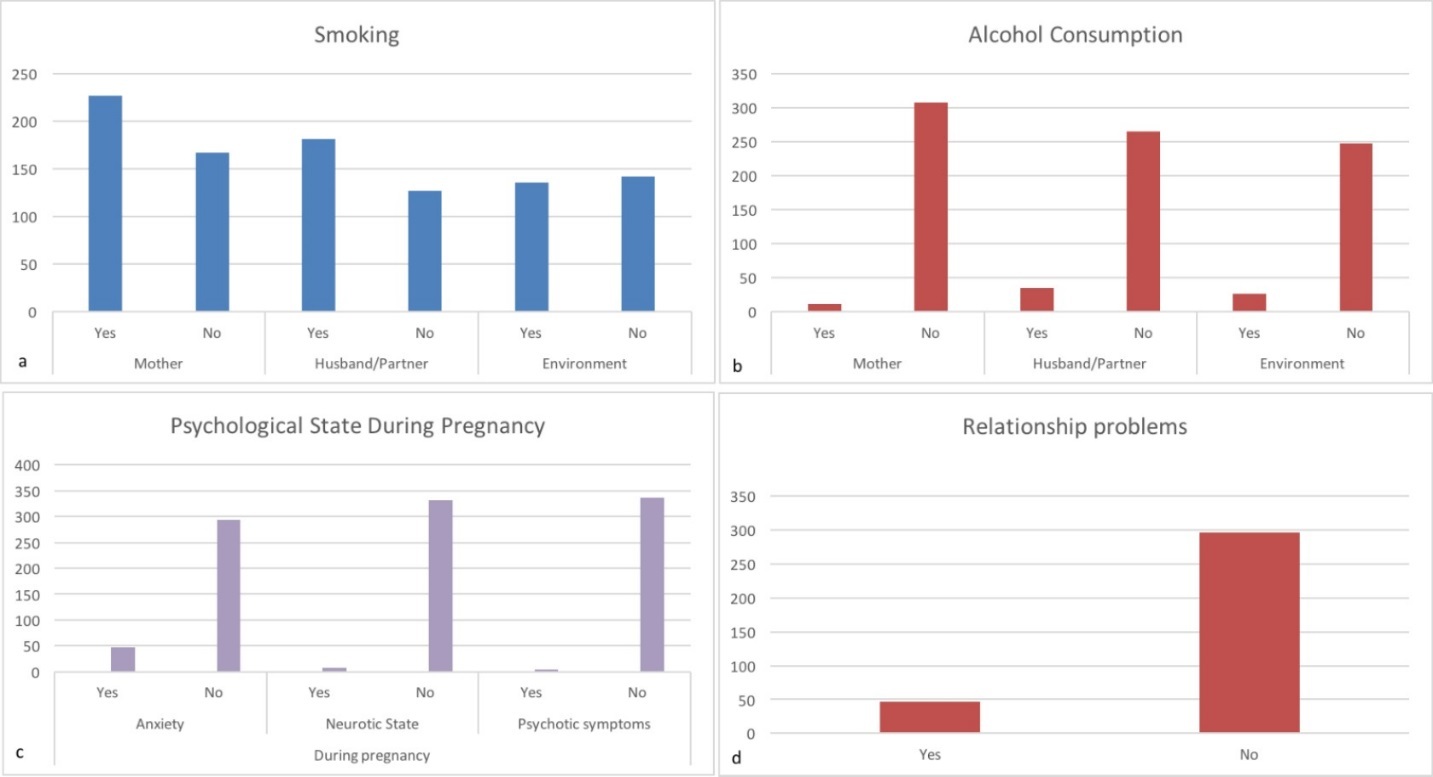
Regarding access to prenatal care services involved in the care of pregnant women from the protective services was for 72 cases (10%), while the obstetrics and gynecology specialist services to 20% (142) were available in the nearest big city (Figure 15). In 16% of cases pediatric services were unavailable in the locality of residence. Social services (family support), child welfare and general practitioners were only available in 10% of cases in the nearest big city.
Figure 15.Accessibility to prenatal care services (If patients had access to health-related services locally or in the neighboring big cities).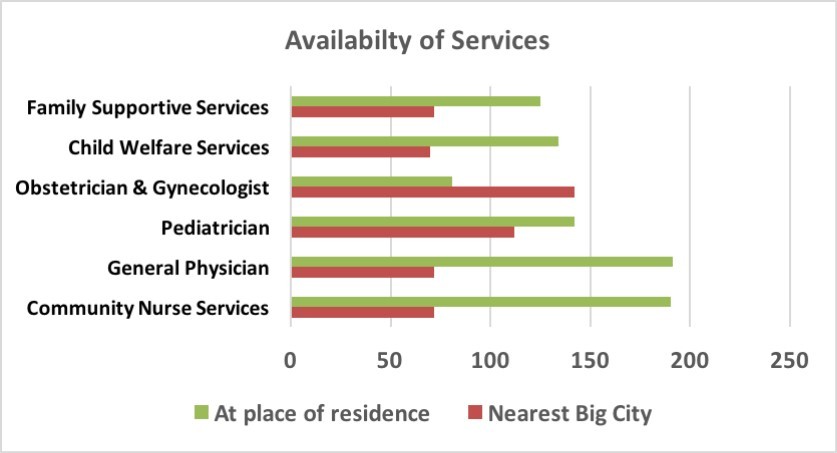
The situation in Hungary in international comparison regarding intrauterine death is not worse (Figure 16). With a death rate of 3.7/1000 we fare better compared to France and Monaco, but majority of European Union countries have better results. Iceland can boast of the best result at (1.3/1000).
Figure 16.Frequency of intrauterine mortality and annual decline in intrauterine mortality in some countries of the world (The Lancet 2016 387, 691-702DOI: (10.1016 / S0140-6736 (15) 01020-X).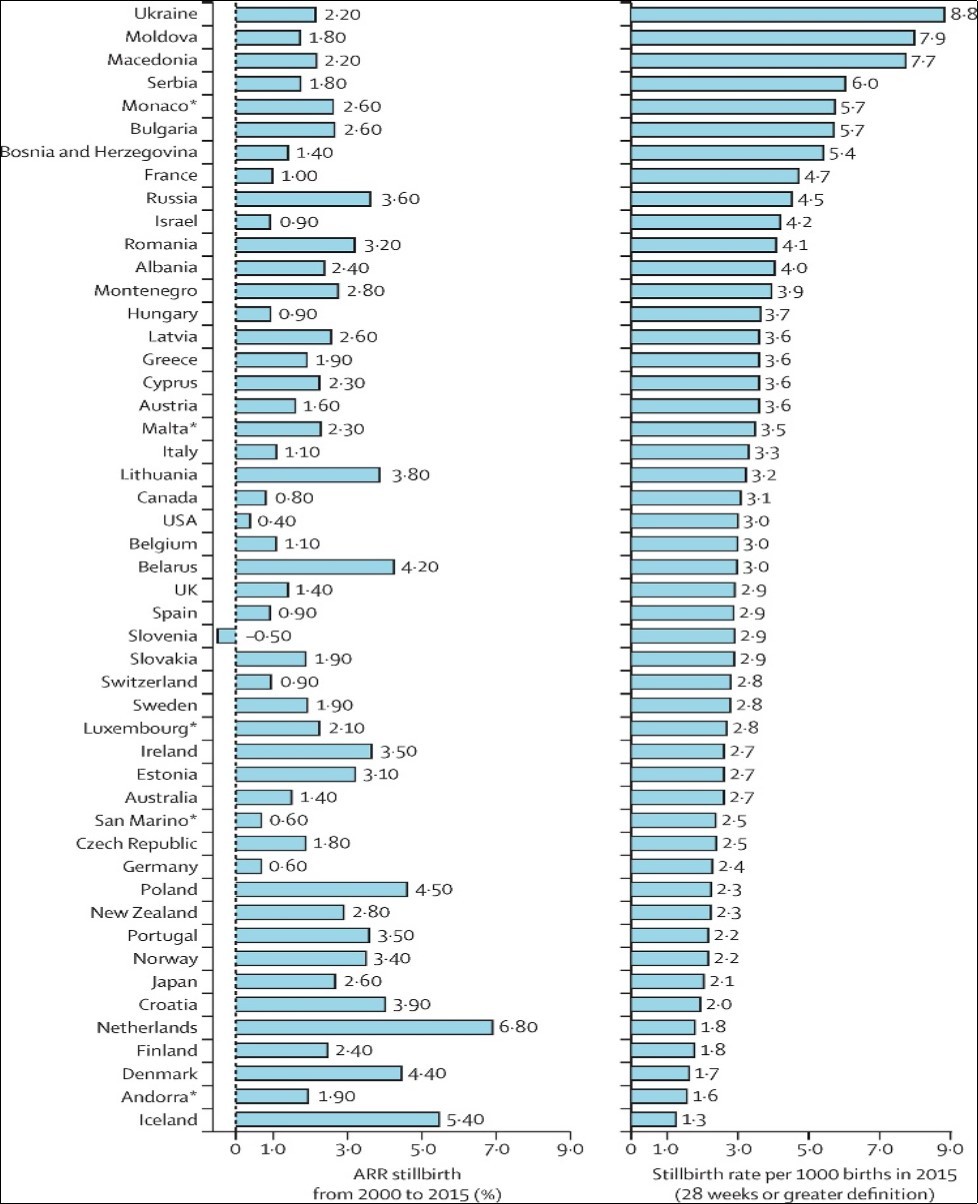
Discussion
Intrauterine death is cumbersome for the spiritual, emotional and physical stress state of the mother. In these cases, the staff involved in this care provision is also spiritually and physically battered 13. The expenditure in the pregnant care networks and hospitals, implemented without years of life can be expressed in profits. The affected families have higher divorce rate and stigmatization of the mothers. The national economy also plays an important role regarding pregnancy 14, birth and child raising by providing financial assistance but in case of intrauterine death cases these cannot be recovered 15. There is evidence to suggest that there is an unacceptable variation in care after stillbirth, and insensitive interactions between staff and bereaved parents 16.
In our case the northeastern counties of the region exceed the national average frequency in case of intrauterine deaths. In this region, 26.8% of the country's population lives and 28% of births take place, but intrauterine death occurs in 35% of the cases. Within this region, the Borsod-Abaúj-Zemplén and Szabolcs-Szatmár-Bereg counties are the most deprived. Unfortunately, like many other economic and social indicators (i.e. income, unemployment, education etc.), from the point of view of the intrauterine death these counties are the most deprived. Borsod-Abaúj-Zemplén and Szabolcs-Szatmár-Bereg counties play a significant role in the incidence of teenage pregnancies in case of intrauterine death. There is a striking correlation between low educational status and the frequency of intrauterine deaths. Between the 24th-36th gestational week 60-80% of the intrauterine deaths take place which reminds us of the importance of strengthening of prenatal care during this period.
In the survey the answers to the raised questions were primarily based on the data collection by nurses. The maternity hospital’s documentation is invaluable regarding pregnant women affected by intrauterine death due to social, economic, housing and health conditions. Most of these women come from areas visited by midwifery services.
Our survey revealed that in more than one-third of intrauterine deaths the cause has been pregnancy related complications (placental abruption and umbilical cord strangulation), whose preventive measures are not yet available in medicine. In 70-80% of cases intrauterine deaths occurred between the 24th and 36th gestational week. In the thesis of Kis-Csitári István PhD, who analyzed the details of intrauterine death and perinatal mortality in the Nógrád county 17. Studies have shown that chronic placental insufficiency monitoring, and pulse oximetry during labor and induction of labor improve perinatal outcomes 18. In our study, strikingly high number of cases were multigravidas and multiparous women. Despite the common antecedents, or risk factors emerging during pregnancy affecting pregnant women show low adherence. This is partly explained by the fact that almost one-third of pregnant women had only primary education. Unemployment (29%) and a significant number requiring social support (20%) is very common among them. 37% of pregnant women lived in apartments without any comforts and furthermore 30% were in inappropriate or neglected hygienic conditions. The risk factor was almost identical to the global survey data 19.
Intrauterine death situation in Hungary compared to international data is not worse (Figure 16). According to the Working Group data of Lancet Stillbirth in High Income Countries which can be compared with the KSH data we are in the middle amongst the developed countries 10, 11. It is noteworthy that regarding both the perinatal mortality and the incidence of intrauterine death Iceland is in the lead. The society’s determination and selfless support towards pregnant women as well as importance of healthy diet is clear, as Iceland has not solved the issue of training doctors and mid-wives play the leading role in pregnancy related care or obstetric care. International studies also draw attention to the underdeveloped regions of expectant financial incentives improving the conditions and can best be persuaded to avail themselves of the opportunities offered by the healthcare system 20. The results of randomized studies of have demonstrated that doubling of pregnant nursing intensity, in addition to various special health education programs (e.g. smoking cessation, nutritional counselling, contraceptive counselling etc.) did not show to decrease in cessation of smoking among teenage pregnancies within 2 years 21. Among pregnancy body weight change, obesity adversely effected intrauterine death frequency and thus, the control of body weight may also play a role in its prevention 22. Randomized studies have shown that cooperation and to improve results so far, the only intervention, the financial incentive („cash incentive”) proved to be the most effective in case of pregnant women in under developed areas 23. Recently the CPIT trial proved that with offered financial incentives for smoking cessation during pregnancy showed a clinically and statistically significant improvement in cessation among pregnant women 24. We are aware of the fact that, after cessation of smoking perinatal outcomes have shown slight improvement 25. Furthermore, in an assessment of 11 studies it was shown that ‘Financial incentives can improve patient compliance’ 26.
Therefore, we would like to presume that through community aid, local bodies support, government or non-profit organizational grants, support provided to women which maybe as minimal as a ‘bus ticket’ to reach an Obstetric care facility, may positively change the trend to a more favorable one not only statistically, but on a broader spectrum emotionally, spiritually and physically and therefore improving the perinatal outcomes.
Conclusion
The changes in the demographic situation in Hungary adversely affects the number of intrauterine deaths. There is currently no sign of a reversal of a negative tendency observed in the incidence of intrauterine deaths on a national scale. In 2015, the twin region of north-eastern Hungary has shown significantly decreased frequency of intrauterine deaths. Therefore, Hungary may be considered in the middle range among developed countries. Among the leading causes placental abruption, umbilical cord complications, chronic placental insufficiency, adverse environmental factors (e.g. social distress, smoking, low education, unemployment) and the lack of co-operation/compliance can be identified.
The proposals to make a positive change in the profession are as follows:
Restoration of Nurses data collection where it was discontinued.
Initiation of interventional studies with regional cooperation.
Strengthening of risk screening and care compliance for pregnant women between the 24th and the 36th gestational week (Travel expenses, e.g. Anticipatory „Bus ticket” for pregnant women, free prenatal vitamins, food aid).
Counting of fetal movements as a screening test.
Cardiotocography (CTG) as a screening test.
Political lobbying to convince financial incentive for care in risk groups.
Reinstitution of Mobile Specialist Services in rural areas where it has been discontinued with appropriate funding from National Health or from local government.
To establish a framework for funding of Doctors and Midwifery home visits.
Importance of advertising of economic and social shelters.
The implementation of the recommendations listed above require policy makers and maintainers to work together, to evaluate the effectiveness and need for additional studies.
Conflict of interests
The authors have no financial interest regarding the study set out in the communication design, conduct, results and conclusions.
Acknowledgements
The authors express their gratitude to all employees involved in the twin region of northeastern Hungary nurse and obstetric and gynecological help in carrying out their work and in regional data collection in the years under review. Special thanks are due to Viziné Kovács Klára, Orbánné Lakatos Judit, Ferenczné Antal Gabriella, Gresó Tiborné, Magyar Veronika dr., Barna Edit dr., Foresz Viktória dr., Teiringer Nóra dr., Bánhidi Andor dr., Váradi Eszter dr., Ditrói Balázs, Simon Zsanett dr. and Csehely Szilvia dr. for their contribution with collection of individual data.
References
- 1.. KSH.(2012november12)Születés körüli halálozások Magyarországon,2011.Statisztikai Tükör. VI.évfolyam88.szám .
- 2. (2016) World Health Organization: Stillbirth a neglected tragedy.http://who.int/maternal_child_adolescent/news_events/better-data-stillbirth-maternal-death/stillbirths-data-1.pdf.
- 3.Balázs P, Rákóczi I, Grenczer A, Foley K L.(Jun2013) Risk factors of preterm birth and low birth weight babies among Roma and non-Roma mothers: a population-based study. , Epub2012Jul18 23(3), 480-5.
- 4.Alio A P, Nana P N, Salihu H M.Spousal violence and potentially preventable single and recurrent spontaneous fetal loss in an African setting: cross-sectional study.
- 5.Janssen P A, Holt V L, Emanuel I, Critchlow C M, Henderson A D.Intimate partner violence and adverse pregnancy outcomes: a population-based study.
- 6.Jejeebhoy S J. (1998) Associations between wife-beating and fetal and infant death: Impressions from a survey in rural India. , Stud fam Plann 29, 300.
- 7.Póka R, Tóth Z. (2015) Az északkelet-magyarországi régió szülészeti és nőgyógyászati tevékenysége és eredményei 2014-ben. , Magy Nőorv L 4, 178-186.
- 8.KSH Gyorstájékoztató Népmozgalom. (2015) Január–december Közzététel:. februáry 23. http://www.ksh.hu/docs/hun/modszgyors/nepmodsz15.html
- 9.KSH.Születés körüli halálozás adatai megyék és a település jogállása szerint.http://statinfo.ksh.hu/Statinfo/haDetails.jsp?query=kshquery&lang=hu.
- 10.KSH.Késői magzati halálozások adatai megyék és a település jogállása szerint.http://statinfo.ksh.hu/Statinfo/haDetails.jsp?query=kshquery&lang=hu.
- 11.Dr Vicki Flenady, Aleena M Wojcieszek, Philippa Middleton BPsySci, Prof David Ellwood.Prof Jan Jaap Erwich, PhD, et al. (February2016)Stillbirths: recall to action in high-income countries. The Lancet Volume 387, Issue 10019. 691-702.
- 12.Zsanett Simon. (2013) Harmadik trimeszterbeli intrauterin magzati elhalások a DEOEC Női Klinikáján 2007-2012 között. Diplomamunka. Témavezető dr.Juhász Alpár Gábor. Debreceni Egyetem Orvos és Egészségtudományi Centrum, Szülészeti és Nőgyógyászati Klinika. , Debrecen
- 13.Heazell Dr Alexander E P, Siassakos Dimitrios, Blencowe Hannah, Christy Burden MRCPCH.Prof Zulfiqar A Bhutta, PhD, et al. (February2016) Stillbirths: economic and psychosocial consequences. The Lancet Volume 387, Issue 10018. 604-616.
- 14.Saleem S, McClure E M, Goudar S S, Patel A, Esamai F.Global Network Maternal Newborn Health Registry Study Investigators. A prospective study of maternal, fetal and neonatal deaths in low- and middle-income countries. doi:. 10-2471.
- 15.Frøen Dr J Frederik, Ingrid K Friberg, Lawn Prof Joy E, Bhutta Prof Zulfiqar A, Robert C Pattinson.(February2016) Stillbirths: progress and unfinished business. doi: 10.1016/S0140-6736(15)00818-1. The Lancet Volume. 387(10018), 574-586.
- 16.Siassakos D, Jackson S, Gleeson K, Chebsey C, Ellis A et al.INSIGHT study group: All bereaved parents are entitled to good care after stillbirth: a mixed-methods multicenter study (INSIGHT). 10-1111.
- 17.Dr,KisCsitáriIstván,„Méhen belüli és a szülés alatti magzati halálozás csökkentésének lehetőségei” Ph.D.értekezés.Ph.D.(2007)program:„A reproduktív endokrinológia nőgyógyászati, szülészeti és neonatológiai aspektusai”, Programvezető:dr.Szabó István egyetemi tanár, a MTA doktora.
- 18.Hedegaard M, Lidegaard Ø, Skovlund C W, Mørch L S, Hedegaard M.Reduction in stillbirths at term and post term pregnancies-results of a national intervention. Danish National Cohort study. 10-1136.
- 19.Lawn Prof Joy E, Hannah Blencowe FRCPCH, Peter Waiswa MRCPCH.Agbessi Amouzou, PhD, Colin Mathers, PhD, et al. (February2016) Stillbirths: rates, risk factors, and acceleration towards 2030. The Lancet Volume 387, Issue 10018. 587-603.
- 20.Bernis Dr Luc de, Mary V Kinney, MSc Prof William Stones, Petra ten Hoope-Bender, Donna Vivio MBA et al.(February2016) Stillbirths: ending preventable deaths by 2030. The Lancet Volume 387, Issue 10019. 703-716.
- 21.Dr Michael Robling, Bekkers Marie-Jet, Bell Kerry, Butler Prof Christopher C, Cannings-John Rebecca.(January2016) Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. , The Lancet 387(10014), 146-155.
- 22.Cnattingius Sven.Eduardo Villamor. (December2,2015) Weight change between successive pregnancies and risks of stillbirth and infant mortality: a nationwide cohort study. Lancet 2016; 387: 558–65. Published Online http://dx.doi.org/10.1016/S0140-6736(15)00990-3
- 23.Pregnancy Cochrane.and Childbirth Group.(31January2015).Incentives for increasing prenatal care use by women in order to improve maternal and neonatal outcomes. doi:. 10-1002.
- 24.McConnachie A, Haig C, Sinclair L, Bauld L, Tappin D M.Birth weight differences between those offered financial voucher incentives for verified smoking cessation and control participants enrolled in the Cessation in Pregnancy Incentives Trial (CPIT), employing an intuitive approach and a Complier Average Causal Effects (CACE) analysis. 10-1186.
