Abstract
Several interactions exist between thyroid and kidney function in many disorders. Many publications explored the relationship between thyroid diseases (TD) and chronic kidney diseases (CKD). However, the morphological thyroid changes in patients with CKD or End Stage Kidney disease (ESKD) were not fully explored. The aim of this study is to explore the morphological and the functional abnormalities of the thyroid gland among ESKD patients as detected by Doppler ultrasound.
Patients and Methods:
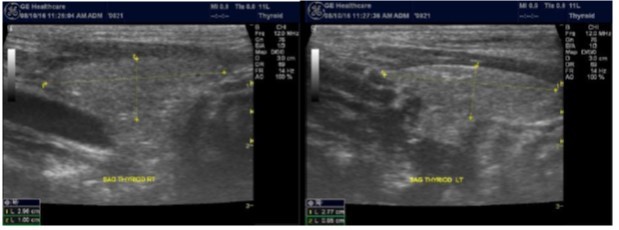
All of the 92 ESKD patients at our center were consented and included in the study. Demographic and clinical data and biochemical and hormonal profiles were recorded. Every patient received a dedicated ultrasound scan of the thyroid gland. GE ultrasound system with Doppler capabilities and high frequency transducer was used. Grey scale imaging and Doppler ultrasound were used to image the thyroid gland for every patient. Taking the thyroid morphology detected by ultrasound and the thyroid function as the dependent variables, all other parameters of age, sex, BMI, occupation, residence, duration of time on dialysis and other comorbilities were taken as independent variables and their relationship to the dependent variables was further studied using appropriate statistical tests.
Results:
Thyroid nodule(s) presence was found to be the most prevalent thyroid morphology detected on ultrasound scanning. Fifty three patients (57.6%) were found to have ultrasound detected nodule(s). The nodule presence was correlated to different independent variables and was found to significantly correlate with age only. The thyroid function as reflected by the level of thyroid hormones was also studied for correlation with the independent variables. No correlation was found between the thyroid function and the presence of nodules.
Conclusion and Recommendation:
Ultrasound detected nodules are very common in ESKD patients. The presence of nodule significantly correlates with patient age denoting its degenerative nature. Ultrasound screening of the thyroid in ESKD patients may be cost effective. However, we recommend a larger multicenter study for better results.
Author Contributions
Academic Editor: Krzysztof Roszkowski, Department of Oncology F. Lukaszczyk Oncology Center Nicolaus Copernicus University
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 O.Osman, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction:
As reported in the literature, there are several interactions between thyroid and kidney function in many disorders 1. Basu etal reported that hypothyroidism is associated with reduced Glomerular filtration rate (GFR) while hyperthyroidism results in increased GFR as well as increased rennin -aldosterone axis activation. They also added that chronic kidney disease (CKD) may be associated with low T3 syndrome 1. CKD patients are also reported to have increased incidence of primary hypothyroidism and subclinical hypothyroidism 2.
Ultrasound Imaging of the Normal Thyroid
The normal thyroid gland consists of two lobes connected with an isthmus 3. The major limitation of ultrasound in thyroid imaging is that it cannot determine thyroid function, i.e. whether the thyroid gland is underactive, overactive or normal in function; for which a blood test or radioactive isotope uptake test is generally required4,5. However, when Doppler US is used, increased gland vascularity may often indicate hyperthyroidism.
Thyroid Ultrasound Examination Technique:
The thyroid gland is examined with neck hyperextended using a high frequency ultrasound transducer, usually in the range of 7-12 MHz, for better resolution. Real time imaging of the thyroid is obtained using both gray-scale and color Doppler techniques. The image characteristics e.g. size, shape, margins, echogenicity, contents and vascular pattern are studied and documented 6, 7.
Normal Thyroid Gland:
The superficial location of the thyroid gland renders it ideal for ultrasound examination 8. High resolution grey scale images can easily be obtained using high frequency transducer. In the transverse view, normal thyroid gland has the butter fly appearance, with left and right lobes connected with a narrow isthmus, Figure 1A. Both lobes can be imaged separately in the longitudinal plan, Figure 1B
Figure 1A.Normal thyroid gland transverse view
Normal Thyroid Volume:
Abnormal Thyroid Scan
Many thyroid abnormalities can be detected by ultrasound. Thyroid pathology detectable by ultrasound can be grouped into focal and diffuse. Thyroid nodules are the most common focal thyroid pathology 11. Diffuse Thyroid pathology includes diffuse of thyroid enlargement as seen in Hashimoto's (lymphocytic) thyroiditis, de-Quervain's subacute thyroiditis, , multinodular goiter and Graves' disease 3. The ultrasonographic features of these pathological entities may be similar but they demonstrate different biochemical and clinical profiles. Accordingly, ultrasound findings should be viewed in the biochemical and clinical context 3.
Thyroid Function Derangement in ESKD Patients
Depending on the GFR, CKD is divided into five stages. The final stages is known as the End stages Kidney disease (ESKD) at which the patient will require renal replacement therapy to sustain life. A disturbance of thyroid function is common in ESRD (End Stage Renal Disease) 12.
Many publications focused on the relationship of thyroid diseases (TD) and CKD. Victoria etal 2 published in 1977 about thyroid dysfunction in chronic renal failure. Then in 2014 Mohamedali etal 13 published about the thyroid disorders and chronic kidney disease. Between Victoria and Mohamedali many publications came out exploring the Interactions between TD and CKD. The example of these publications is given by what have been published by Lim VS in 200114; P Iglesias etal in 200915 and Gopal Basu etal in 20121. However, most published data dealt mainly with the functional relationship between TD and CKD; in this study the morphological abnormalities of thyroid among ESKD as detected by Doppler ultrasound imaging were also explored.
Patients and Methods
The main objective of this study is to examine the morphological and functional abnormalities of the thyroid gland among ESKD Patients. To achieve this objective, all the 92 chronic hemodialysis patients at Prince Sultan Kidney Dialysis Center at Alqunfudah general hospital were consented and included in the study. All patients underwent thyroid ultrasound scanning. Grey scale imagings were obtained first followed by Doppler interrogations. GE ultrasound system with high-resolution linear probe (7.5-12 MHz) and advanced scanning techniques like extended field of view and compound harmonic imaging were applied to get the best image quality. Demographic and clinical data were recorded for all patients in addition to chemical and hormonal laboratory results. The collected data was processed and analyzed to satisfy the objectives of the study. The categorical data was presented as frequency and percent. The continuous data was presented in terms of mean and standard deviation. X2 test was used for categorical data, student t-test was used for continuous data. To better study the relationship between the dependant and the independent variables, logistic regression was used to study all the possible directions of the association between the dependant and the independent variables.
Results
The sample population is composed of 50 (54.3%) male and 42 (45.7%) female mirror image the male dominance of kidneys diseases, Table 1. The age of the participants falls in the range of 15-85 years with a mean of 54.6 years and a median of 60 years denoting the degenerative nature of ESKD with incidence increases with age. Table 2.
Table 1. shows the gender percentage of the patients| Cumulative Percent | Valid Percent | Percent | Frequency | |
| 54.3 | 54.3 | 54.3 | 50 | male |
| 100 | 45.7 | 45.7 | 42 | Female |
| BMI | HEIGHT | WEIGHT | AGE | |
| 91 | 91 | 91 | 91 | Valid |
| 1 | 1 | 1 | 1 | Missing |
| 22.4109 | 156.18 | 55.236 | 54.62 | Mean |
| 21.5188 | 156 | 55 | 60 | Median |
| 5.55904 | 12.382 | 16.5624 | 16.475 | Std. Deviation |
| 12.86 | 110 | 18.5 | 15 | Minimum |
| 42.24 | 185 | 115 | 85 | Maximum |
The presence of nodule(s) was found to be the most common morphology detected by ultrasound among the study cohort, Table 3
The mean age of those with nodules is higher (59.66 years) than the mean age of those without nodules (47.68 years). The differences was found to be statistically significant (P = 0.001) denoting also the degenerative nature of thyroid nodules, Table 3.
Table 3. shows that the presence of nodule(s) significantly increases with age| Std. Error Mean | Std. Deviation | Mean age | N | Nodule |
| 2.099 | 15.281 | 59.66 | 53 | Nodule present |
| 2.714 | 15.828 | 47.68 | 34 | No nodule |
When the relationship between the presences of nodule is studied versus the other demographic variables (age, sex, height, weight, BMI, occupation, family size and residency), it was found to significantly correlate with age (P. = 0.024). No significant correlation was found between the presence of nodule and other demographic variables. In contrary to the fact that thyroid diseases are more common in female, no significant variation in nodules presence was found with sex.
Also no significant correlation was found between the presence of nodule and other comorbidies (diabetes, hypertension and other comorbidities) or between the presence of nodule and the duration of time on dialysis in months.
The presence of a thyroid nodule significantly correlated with CRP (P=0.014) when t- Test was used. However, when this relation was further scrutinized using logistic regression, it was not found significant. .No significant correlation was found between the presence of nodule and other biochemical parameters (ESR, Phosphate, Calcium, ALP and thyroid and parathyroid hormones), Table 4. The relationship between the nodule presence and the virus status of the participants was also studied but no significant correlation was found, Table 5.
Table 4. Shows the Biochemical and hormonal variations of the patients| CA | PHOSPH | PTH | ALP | T3 | T4 | ESR | CRP | |
| Valid | 91 | 91 | 91 | 89 | 87 | 87 | 77 | 81 |
| Missing | 1 | 1 | 1 | 3 | 5 | 5 | 15 | 11 |
| Mean | 7.944 | 4.788 | 832.76 | 168.8 | 4.3983 | 11.662 | 58.9 | 8.59 |
| Median | 8.1 | 4.7 | 628 | 102 | 4.28 | 11.59 | 60 | 6 |
| Std. Deviation | 0.9576 | 1.6702 | 809.958 | 202.956 | 0.94357 | 2.4485 | 38.757 | 5.995 |
| Minimum | 5.5 | 0.9 | 7 | 36 | 2.38 | 4.8 | 3 | 6 |
| Maximum | 9.8 | 10.3 | 4055 | 1270 | 8.5 | 17.9 | 138 | 24 |
| Frequency | Percent | Valid Percent | Cumulative Percent | |
| Negative | 73 | 79.3 | 80.2 | 80.2 |
| C | 15 | 16.3 | 16.5 | 96.7 |
| B | 3 | 3.3 | 3.3 | 100 |
| Missing | 1 | 1.1 | ||
| Total | 92 | 100 |
1.Also no significant difference was found in the presence of thyroid nodule among those who reported thyroid disease symptoms and/or signs and those who did not.
Discussion
The reported prevalence of nodular thyroid disease depends on the population studied and the methods used to detect nodules 16. Our study population is unique as it is composed entirely of ESKD patients. We also used ultrasound as a method of detecting thyroid abnormalities. In our study the prevalence of thyroid nodular pathology as detected by ultrasound was found to be 57.6% mirror image what reported in the literature as it has been reported that nodules found on ultrasonography suggest a prevalence of 19 to 67%17, 18; and in other publications it has been reported to range from 50% to 70% 7, 8. Figure 3A below shows an Ultrasound detected thyroid nodule.
The prevalence of thyroid nodule is also influenced by age. In one study, 30 % of subjects 19 to 50 years of age had an incidental nodule on ultrasonography19. However, from our work we found that the presence of nodules increases with age. This may explain the reported low incidence of thyroid nodule in the age group 19-50 years. Also, with the widespread use of sensitive imaging in clinical practice, incidental thyroid nodules are being discovered with increasing frequency.
High-resolution ultrasonography (USG) is the most accurate and cost-effective method for evaluating and observing thyroid nodules 3. Although there is some overlap between ultrasound appearance of benign and malignant nodules, certain USG features are helpful in differentiating the two. Iso-or hyper-echogenicity of the thyroid nodule in conjunction with a spongiform appearance is the most reliable criterion for benignity of the nodule on gray-scale ultrasound, Figure 4A. Other features like nodule size <1 cm, width > length, presence of hypoechoic or hyperoechoic halo around the nodule, Figure 4A and Figure 4B, caused by fibrous capsule compressing thyroid tissue, and coarse/curvilinear calcification are less specific but may be useful ancillary signs4 ,6. "Ring down" or "comet-tail" artifact or sign is typical of benign cystic colloid nodule, Figure 520. Perinodular flow or spoke-and-wheel-like appearance of vessels on color Doppler examination is characteristic of a benign thyroid nodule. However, this flow pattern may also be seen in thyroid malignancy. A complete avascular nodule is very unlikely to be malignant 4.
Figure 4B.Isoechoic nodule with Hyperechoic rim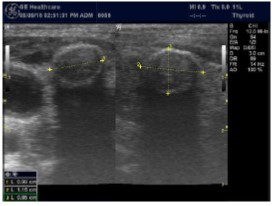
Figure 5.Ring down artifact of colloid nodule
Malignant focal thyroid pathology
Thyroid cancer is classified according to the histological appearance into papillary carcinoma (60-80%), follicular carcinoma (20-25%), medullary carcinoma (4-5%), anaplastic carcinoma (3-10%), lymphoma (5%) and metastases21. Thyroid ultrasound is reported to have overall sensitivity of 83.3% in diagnosing a malignant nodule 7. Ultrasound features predictive of malignant nodules include presence of microcalcifications , marked hypoechogenicity, irregular margins, local invasion, lymph node metastases, solid composition, absence of a hypoechoic halo around the nodule, size >1 cm, taller-than-wide-shape, and an intra nodular vascularity 22. Unlike what is popularly known, multiplicity of the nodule is not an indicator of benignity. The incidence of malignancy is same in solitary nodules as it is in multiple nodules 3.
Any nodule with intermediate indeterminate cytology or higher on FNA should go to surgery 23. Among our patients population, one patient with nodular pathology and tertiary hyperparathyroidism was found to have papillary carcinoma of the thyroid during parathyroiectomy. Total thyroidecotmy was done and the patient got forearm implantation of one of the parathyroid glands, Figure 6.
Figure 6.Total thyroidecotmy and forearm implantation of the parathyroid gland
Some experts prefer partial or total thyroidectomy if the cancer is already confirmed before
surgery. However, no consensus exists about partial thyroidectomy 23. Some authors recommend ablation using radioactive iodine (I-131) for high-risk patients with postoperative thyroid replacement therapy but the benefits of administration remain controversial in low-risk patients 23, ,24. Follow up with regular TSH is recommended following complete resection of thyroid cancer. The TSH concentration should be in the target range of 0.5 μU per mL. Greater suppression may be necessary for high-risk patients and those with a metastatic or locally invasive tumor.
In our study we also found that nodule presence significantly increases with age (P. Value .024) going along with what is been published by Vikas Chaudhary, et al 3. He reported that” Nodule incidence increases with age, and is increased in women, in people with
iodine deficiency, and after radiation exposure”. However, in our study we could not detect any significant relations with other variables like sex, and Phosphate. We found that CRP significantly correlates with nodule using t-test but not when logistic regression analysis was used. Should the correlation proven to be significant; it would not be difficult to explain it in light of the fact that inflammation may potentiate degeneration. However, dedicated study to address the issue is needed.
Parathyroid Glands Pathology:
In our study many patients were found to have nodules look very much like PT adenoma, Figure 7 below. At least, 4 patients were subsequently confirmed to have parathyroid adenomas, Figure 8 and 2 patients underwent surgery
Despite the fact that nodular pathology was found to be very prevalent among our study population, it has been found difficult to differentiate between thyroid and parathyroid pathology using ultrasound alone. However, some characteristics of the parathyroid glands might suggest parathyroid pathology in the context of the clinical picture of secondary or tertiary hyperparathyroidism which is very prevalent in ESKD patients’ populations.
Figure 7.Thyroid nodule suspicious for Parathyroid adenoma due to its location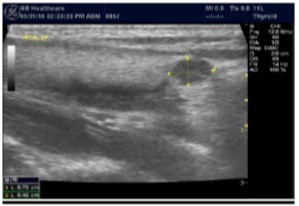
Figure 8.Nodule that proven to be a parathyroid adenoma, volume =5265 mm3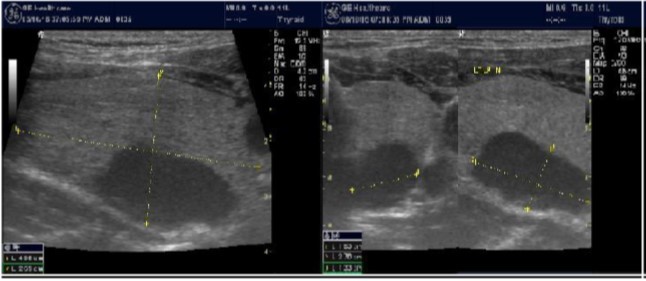
There are 4 parathyroid glands (2 superior, 2 inferior) imbedded within the thyroid gland. The parathyroid glands are bean-like shape and small (20-40 mg) 25. Sonographically, the parathyroid glands have the following features 25:
Normal glands: indistinguishable from thyroid parenchyma.
Hyperplastic glands: hypoechoic, volume <500 mm3.
Nodular glands: hypoechoic. Volume >500 mm3
Histologically, if the excised gland has volume <500 mm3 it is said to be hyperplastic and if the volume is more than 500 mm3 it is nodular hyperplasia in 80% of cases26. In secondary HPT, the increase in the volume of parathyroid glands is associated with increase in vascularity, as evident in Color Doppler imaging 27.
Conclusion
Despite the fact that nodular pathology of the thyroid is prevalent among ESKD patients, the prevalence was not different from what reported for the general population. Ultrasound imaging is cost effective in detecting nodular thyroid pathology.
However, ultrasound will not differentiate between thyroid and parathyroid pathology. It is also limited in differentiating benign from malignant pathology. These limitations may be overcome by adding Sestamibi parathyroid scan and FNA, respectively.
Recommendations
We recommend all ESKD patients on dialysis to have annual thyroid ultrasound scan. We also recommend a large multicenter study for better results.
References
- 1.Basu Gopal, Mohapatra Anjali. (2012) Interactions between thyroid disorders and kidney disease; Indian J Endocrinol Metab. , Mar-Apr; 16(2), 204-213.
- 2.Victoria Sy Lim.Thyroid Dysfunction in Chronic Renal Failure;. , J Clin Invest.Sep1977; 60(3), 522-534.
- 4.Solbiati L, Charboneau J W, Osti V, James E M, Hay I D. (2005) The thyroid gland. In: Rumack CM,Wilson SR,Charboneau JW,Editors. Diagnostic Ultrasound. 3rd ed.,Vol.1.St.Louis,Missouri:Elsevier Mosby. 735-70.
- 5.Chaudhary V, Bano S. (2012) Imaging of the thyroid: Recent advances. , Indian J Endocrinol Metab 16, 371-6.
- 6.Baskin H J. (2007) Ultrasound of thyroid nodules. In: Baskin HJ,Editor. Thyroid Ultrasound and Ultrasound-guided FNA Biopsy. 71-86.
- 7.Moon W J, Jung S L, Lee J H, Na D G, Baek J H et al. (2008) Benign and malignant thyroid nodules: US differentiation–multicenter retrospective study. , Radiology 247, 762-70.
- 8.Dobruch-Sobczak Katarzyna, Jędrzejowski Maciej, Jakubowski Wiesław, Trzebińska Anna.Errors and mistakes in ultrasound diagnostics of the thyroid gland;J Ultrason.Piblishedonline2014Mar30;. 14(56), 61-73.
- 10.Delange F, Benker G, Caron P. (1997) Thyroid volume and urinary iodine in European schoolchildren: standardization of values for assessment of iodine deficiency. , Eur J Endocrinol 136, 180-187.
- 12.Fa Sarvghadi, Sa Khalili, Ab Tara, Jc Najafi, Aa Aliasgari et al. (2007) Thyroid Function and Volume Changes. in Patients E with End Stage Renal Disease, Before and After Kidney Transplantation. Int J Endocrinol Metab 3, 141-148.
- 13.Mohamedali Mohamed.Srikanth Reddy Maddika, Anix Vyas, Viswanathan Iyer, and Pramil Cheriyath; Thyroid Disorders and Chronic Kidney Disease;. , International Journal of Nephrology.Volume2014(2014),ArticleID520281,6pages
- 14.Lim V S.Thyroid function in patients with chronic renal failure;. , Am J Kidney Dis.2001Oct.38(4Suppl1) 80, 4.
- 15.Iglesias P, Díez J.Thyroid dysfunction and kidney disease;. , Eur J Endocrinol April1,2009 160, 503-515.
- 16.Dean D S, Gharib H.Epidemiology of thyroid nodules. , Best Pract Res Clin Endocrinol Metab.2008Dec; 22(6), 901-11.
- 18.Tan G H, Gharib H. (1997) Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. , Ann Intern Med 126, 226-31.
- 19.Brander A, Viikinkoski P, Nickels J, Kivisaari L. (1991) Thyroid gland: US screening in a random adult population. , Radiology 181, 683-7.
- 20.Ahuja A, Chick W, King W, Metreweli C. (1996) Clinical significance of the comet tail artifact in thyroid ultrasound. , J Clin Ultrasound 24, 129-33.
- 21.Brkljaciæ B, Cuk V, Tomiæ-Brzac H, Bence-Zigman Z, Deliæ-Brkljaciæ D et al. (1994) Ultrasonic evaluation of benign and malignant nodules in echographically multinodular thyroids. , J Clin Ultrasound 22, 71-6.
- 22.Hoang J K, Lee W K, Lee M, Johnson D, Farrell S. (2007) US Features of thyroid malignancy: Pearls and pitfalls. , Radiographics 27, 84760.
- 23.Shaha A R. (2000) Controversies in the management of thyroid nodule. , Laryngoscope 110(2 Pt 1, 183-93.
- 24.Singer P A, Cooper D S, Daniels G H, Ladenson P W, Greenspan F S et al. (1996) Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. , Arch Intern Med 156, 2165-72.
- 25.Mario Petrucci Meola, Cupisti Ilaria, Adamasco. (2013) Ultrasound in clinical setting of secondary Hyperparathyroidism. , JNEPHROL 26(5), 848-855.
- 26.Périé S, Fessi H, Tassart M. (2005) Usefulness of combination of high-resolution ultrasonography and dual-phase dual-isotope iodine 123/technetium Tc 99m sestamibi scintigraphy for the preoperative localization of hyperplastic parathyroid glands in renal hyperparathyroidism. , Am J Kidney Dis 45(2), 344-352.