Postulation of the Effect of Unpredicted Predisposing Factors for Post-Tonsillectomy Bleeding
Abstract
Back ground and Objectives
Tonsillectomy is the most common surgical procedure in specialty of otorhinolaryngology. Therefore there are frequent premises regarding this procedure to be improved from different aspects, indications, time of surgery, techniques, safety measures, and postoperative care. Hence the tonsils and peritonsillar tissues are highly vascular zone that supplied by direct branches of external carotid artery thus the post-tonsillectomy bleeding remains one of significant issues in relation to this widely performed procedure. The post-tonsillectomy bleeding needs frequently to be postulated for its incidence, prevalence, etiology, predisposing factors, management and prevention. This subject constitutes one of most risky aspects that increase wariness of the surgeons regarding this commonly conducted procedure. Although there are huge numbers of presentative literatures coming from American as well as western institutes that tried to put guidelines for purpose of prevention and management of post-tonsillectomy bleeding but broadly at our middle-east region and locally at our Libyan society we found for some extent difficulties to apply all these guidelines. For this reason this issue has been take the wider spectrum of ENT surgeons’ concentration, discussions, and researches.
Therefore this study was conducted prospectively and for long time to confirm the possible predisposing factors that could be responsible for increasing the risk of post-tonsillectomy bleeding at our region and in the same time to illustrate the concluded recommendations to prevent the occurrence of this important complication.
Patients and Methods
2880 patients aged from 8 months to 85 years presented at ENT department-AL-hawari ENT and urology teaching center- Benghazi-city – Libya as well as AL-thowra central teaching hospital and AL-tarahom private center – Elbyda city – Libya at period in between September 2003 to March 2015 as cases of chronic adeno-tonsillitis and solitary acute as well as chronic related palatine tonsillar disease with variable patterns of indications for tonsillectomy namely snoring and apnea attacks, recurrent attacks of acute tonsillitis, persistent otitis media with effusion, recurrent attacks of acute suppurative otitis media, failure to thrive, recurrent attacks of chest infection, mal-occlusive dental deformity, unilateral enlarged tonsils, post-traumatic avulsed tonsils, history of quinsy abscess and persistent halitosis. All patients were assessed intra-operatively and post-operatively too for any evidences of primary, reactionary, or secondary hemorrhage in relation to wide spectrum of factors as patient's demographic, medical, and socio-habitual factors, in addition to technical as well as post-operative care factors.
Results
This presenting study confirmed that the most common type of post-tonsillectomy bleeding was the secondary variety (71%) as compared to primary (22%) and reactionary (7%) among all presented post-tonsillectomy bleeding cases. Although through this presenting serial study there were multifactorial pre-dispositions elucidated for secondary post-tonsillectomy hemorrhage but as general poor post-operative care can be considered as the cornerstone for the pathogenesis of this significantly raised incidence of secondary post-tonsillectomy bleeding this may be in form of inadequate patient's hydration and nutritional supply (47%), poor patient's antibiotic compliance (23%), and child's maternal negligence (19%). The time of surgery was found to be another important pre-disposing factor for post-tonsillectomy bleeding, it was postulated that the incidence of reactionary as well as secondary post-tonsillectomy hemorrhage significantly increased at summer and autumn seasons (69%) as compared to other seasons. The place of surgery was another interesting proposed studied factor among this serial presentation it was observed that the incidence of post-tonsillectomy bleeding among patients who operated at AL-hawari ENT and urology teaching center-Benghazi-city significantly higher (63%) than that among cases who interfered at AL-thowra central teaching hospital and AL-tarahom private center – Elbyda city.
Conclusion
Generally speaking, post-tonsillectomy bleeding is considered as one of important issues in ENT and one of significant post-tonsillectomy complications which may create a critical morbidity that may rarely extend to post-operative mortality. Hence the most common pattern of post-tonsillectomy bleeding is the secondary type; however this type of post-tonsillectomy hemorrhage is pre-disposed and induced by many factors. Most of these factors are treatable and curable thus the prophylaxis against this significant complication can be achievable.
Author Contributions
Academic Editor: Jon Ver Halen, Dept of Plastic and Reconstructive Surgery Baptist Cancer Center 3268 Duke Circle Germantown, TN 38139.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Khaled Mohamed Bofares
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Post-tonsillectomy bleeding (PTB) is considered as one of important issues at otorhinolaryngology which frequently speeds much time and effort for research activities due to its relation to most commonly performed procedure that is the tonsillectomy and hence PTB may create critical morbidities that may rarely extend to post-tonsillectomy death thus there will be always clinical trials to study the types, predisposing factors, causes, and suggestions for prevention and management of this significant complication 1, 2, 3, 4, 5, 9, 10, 11, 12, 13. Although there is wide spectrum of indications for tonsillectomy but among of all these indications there are certain conditions which may be associated with increased risk of PTB for instance the cases of previous quinsy abscess, tonsillar malignancy, acutely infected tonsils, and uncontrolled hemorrhagic tonsillitis 1.
In addition, there are variable post-tonsillectomy complications which range between systemic to local, and early to late as complications of general anesthesia, aspiration to the lungs, negative pressure pulmonary edema, air way obstruction, local traumas, remnant tonsil, local infection, velopharyngeal dysfunction, and nutritional deficiencies 10,15. Also all the complications of tonsillectomy can be discussed on the basis of their relation to PTB i.e. some of these complications have direct relation to PTB by their classification as significant etiologies for PTB as the local iatrogenic soft tissue traumas and local infection. In accordance, the other complications have opposite direct relation to PTB by the action of PTB as one of common predisposing factor for these complications as aspiration to the lungs, air way obstruction due to laryngospasm or large clot formation, chest infection, respiratory failure, cardiovascular shock, and disseminated intravascular coagulopathy. From the other view, there is other group of post-tonsillectomy complications which can be aggravated by PTB resulting in raised morbidity and mortality rates as dehydration, metabolic disturbances, and nutritional deficiencies 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23.
Although there are three varieties of PTB, primary, reactionary, and secondary but the most common pattern is the secondary PTB as concluded by several previous studies 24, 25, 26, 27. This can be correlated to the improvement of tonsillectomy procedure recently from the patients' pre-operative care as well as the technology point of views resulting in low incidence of primary and reactionary PTB 24, 25, 26, 27. In accordance, hence the secondary PTB had been confirmed to be mainly due to the post-operative local infection thus there are multifactorial predispositions which may act as significant causes for post-operative infection at the tonsillar fossae as well as the peri-tonsillar area and subsequently the occurrence of secondary PTB. From the patient's age point of view, as it is well-established that the children with PTB will be at serious situations as compared to adults therefore the poor maternal post-operative care for the operated child can be considered as one of important predisposing factors for secondary PTB i.e. the negligence of child regarding maternal encouragement for early oral fluids and soft diets can be described as the cornerstone for child dehydration which leads to increased infective activity of local opportunistic flora due to reduced secretory immune capacity of the saliva by two mechanisms, first by decreased secretion rate of IgA through reduced saliva volume and the second by significant change of saliva PH. In addition, the poor sanitation as well as poor child's hygiene among low social class families with limited maternal education can be considered as other predisposing factors that may act toward the facilitation of pathogenesis of local infection 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27.
On the other hand, there are other causes which can be categorized as important etiologies for PTB as bleeding disorders, remnant tonsillar tissue, stitch granuloma, local traumas, slipping of ligatures, diffuse fibrosis with difficult dissection, and pharyngo-laryngeal reflux but now days all these causes became of less significance by the improvement of pre-operative patient evaluation in addition to recent advancements as well as the developments in relation to tonsillectomy techniques. Although in spite of these improvements the incidence of secondary PTB is still found to be high thus the researching activities had been directed for assessment of postoperative conditions to postulate what could be the predisposing factors that responsible for the increased incidence rate of secondary PTB 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37.
From our clinical observations at our Middle East society, we noted that the social as well as habitual factors are considered as another significant variety of secondary PTB predisposing factors. The maternal education, socioeconomic status, sanitation as well as hygiene conditions, and patients' psychological status were elucidated to play a significant effect on the incidence rate of secondary PTB. In addition, there are other co-morbid conditions with the palatine tonsillar disorders that may increase the risk of secondary PTB as uncontrolled allergic rhinitis as well as gastro-esophageal reflux disease (GERD). Thus this serial study was planned to achieve these aims:
To assess the effect of maternal education level on the secondary PTB incidence rate among operated children.
To postulate the effect of maternal and patients' psychological status on the secondary PTB incidence rate among operated children as well as adult patients consecutively.
To elucidate the effect of sanitation and hygiene conditions on the secondary PTB incidence rate among operated patients.
To confirm the effect of socioeconomic status on the secondary PTB incidence rate among operated patients.
To illustrate the effect of co-morbid disease conditions namely allergic rhinitis and GERD on secondary PTB incidence rate among operated patients.
Patients and Methods
As prospective study, 2880 patients aged from 8 months to 85 years presented at ENT department- AL-hawari ENT and urology teaching center- Benghazi-city – Libya as well as AL-thowra central teaching hospital and AL-tarahom private center – Elbyda city – Libya at period in between September 2003 to March 2015 as cases of chronic adeno-tonsillitis and solitary acute as well as chronic related palatine tonsillar disease with variable patterns of indications for tonsillectomy namely, snoring and apnea attacks, recurrent attacks of acute tonsillitis, persistent otitis media with effusion, recurrent attacks of acute suppurative otitis media, failure to thrive, recurrent attacks of chest infection, mal-occlusive dental deformity, unilateral enlarged tonsils, post-traumatic avulsed tonsils, history of quinsy abscess and persistent halitosis. All patients were operated by dissection method and bleeding control was by pack pressure as well as electrical cauterization. All patients were assessed intra-operatively and post-operatively too for any evidences of primary, reactionary, or secondary hemorrhage in relation to wide spectrum of unpredicted factors namely, patients' socio-economic, habitual, sanitation, housing, and hygiene factors. In addition, the patients' medical status namely severity of co-morbid allergic rhinitis as well as pharyngo-esophageal reflux and uncontrolled psychiatric status were considered as other significant factors which also evaluated in relation to incidence of PTB. Informed consents were taken from the parents of all operated children or from adult patients themselves involved in the research prior to their participation.
Data were expressed by using descriptive analysis as means + standard error of mean (s. e. m) and percentages, test of significance was curried out, using Chi-squar test and two way analysis of variance. A probability less than 0.05 was considered as significant, the degree of significance was determined by using level of standard deviation test. Student-t-test was used for dependent sample, as well as contingency coefficient was calculated as measurement of association between nominal variable.
Results
The Figure 1 showed significant raising of the incidence of secondary PTB among operated children who cared by poorly educated mothers as compared to those who are under postoperative care by well-educated mothers (P < 0.1). Figure 2 illustrated significant elevation of the incidence of secondary PTB among operated children with psychiatrically abnormal mothers as well as among adults who are known cases of variable psychiatric problems (P < 0.1). On the other hand, Figure 3 demonstrated that there is significant increase of the incidence of secondary PTB among operated patients who are living with big sized families (family members > five) as compared to others (P < 0.1). In accordance, Figure 4 represented that the incidence of secondary PTB was significantly increased among operated patients who have poor sanitation at their houses as compared to those with good sanitation (P < 0.1). In addition Figure 5 demonstrated significant elevation of the incidence of secondary PTB among patients with low socioeconomic status as compared to others (P < 0.1). From the other view, Figure 6 and Figure 7 showed significant increase in the incidence of PTB among patients with co-existing uncontrolled allergic rhinitis and uncontrolled GERD consecutively (P < 0.1).
Figure 1.The relationship between maternal education level and PTB incidence rate among operated children (P < 0.1).
Figure 2.The effect of maternal and patients' psychological status on the PTB incidence rate among operated children as well as adult patients consecutively. (N= normal psychological status, N.D= neurotic disorders, M.D= manic disorder, D.D= depression disorder, S.PH.D= schizophrenic disorder), (P < 0.1).
Figure 3.The relationship between patient's family members number (<5, 5, and >5 members) and PTB incidence rate among operated children (P < 0.1).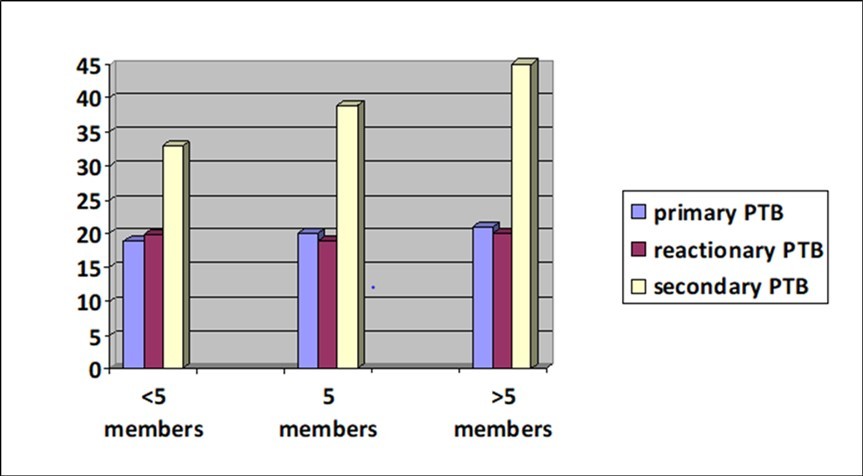
Figure 4.The relationship between sanitation status good sanitation= family members < five members and house with > two rooms poor sanitation= family members ≥ five members and house with ≤ two rooms and PTB incidence rate among operated patients (P < 0.1).
Figure 5.The relationship between patients' family economic status high salary= >2500LD (~ >1000$) medium salary= 1000 and PTB incidence rate among operated patients (P < 0.1).
Figure 6.The relationship between co-existence of allergic rhinitis and PTB incidence rate among operated patients (P < 0.1). NAR=no allergic rhinitis CAR=controlled allergic rhinitis and NCAR=uncontrolled allergic rhinitis.
Figure 7.The relationship between co-existence of GERD and PTB incidence rate among operated patients (P < 0.1).
Discussion
Although by the progress of the sciences and further development of the surgical technology at this presenting century; still the incidence of PTB is significantly high24, 25, 26, 27.. This can be shown via several well- controlled clinical studies. This means that there are other possible suggested factors rather than technical or medical factors which could play a significant role regarding predisposition for PTB. Hence the secondary PTB constitutes most common variety as compared to primary and reactionary thus this confirm that the technical as well as the medical factors have minimal consideration as etiological factors for PTB because these factors had been elucidated to be bothersome factors of primary and reactionary PTB. Therefore it becomes very necessary to research and illustrate for other possible predisposing factors 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32.
At this serial clinical prospective study we suggested a cluster of certain new pattern of factors which could be unpredicted. This manner of factors is more related to social status of the patients rather than their demographic or medical criteria. In accordance and from our clinical observations we noted that these unpredicted groups of factors play a very significant role in estimation of incidence rate of secondary PTB. The education level of operated child's mother can be considered as one of these important factors it was elucidated that the improvement of maternal as well as patient education level will reduce significantly the incidence rate of secondary PTB among operated children and adults consecutively. This can be correlated to the degree of post-operative care in relation to the education level i.e. the improvement of education level will be reflected positively on the maternal and patient understanding for the importance of encouragement for early oral feeding by cold fluids as well as soft diets, restricted compliance for post-operative prescribed medication administration particularly analgesics as well as antibiotics, and post-operative close observations regarding persistent fever, repetitive vomiting, , latency, fatigability, malaise, persistent dysphagia, persistent odynophagia, and PTB 33, 34, 38, 39.
On the other hand, the maternal as well as patients' psychological status was affecting significantly the incidence rate of secondary PTB among operated children and adult patients consecutively. This can be explained by the increase of post-operative negligence and carelessness proportionally with worseness of co-existing psychological disorders. The mothers with manic, depressant, or schizophrenic psychotic disorders had been shown poor compliance regarding frequency of post-operative fluids and soft diets administrations to their operated children; in addition those mothers had been presented significantly a higher rate of post-operative analgesics as well as antibiotics missing to their operated children. The same observations were elucidated among operated adults with manic, depressant, or schizophrenic psychotic disorders. Therefore this can result in significant rising of secondary PTB as predisposed by uncontrolled dehydration and infection.
From the other view, there is another unpredicted and masked predisposing factor for secondary PTB which is the sanitation and hygiene status of the environment where the operated patient is living. From the primary health care point of view, the sanitation status can be classified on basis of number of family members in relation to their house rooms number into two categories, good sanitation which is defined by family members number less than five who are living at house contains more than two rooms, and poor sanitation which is indicated by family members number of five or more who are living at too small house that composed of two rooms or less. The presented study postulated that the incidence rate of secondary PTB was significantly increased among operated patients who are living at poor sanitation. This can be reasoned by the increase of incidence rate of post-tonsillectomy infection at environments with poor sanitation due to overcrowding as well as bothersome negligence, carelessness and bad hygiene. In accordance, it was found that if the operated child living with both parents this shown significantly decreased incidence rate of secondary PTB as compared to the other situations when the operated child living with one parent or other relatives rather than parents as grandfather, grandmother, uncle, or aunt.
At developing countries there is another factor which could be suggested as important unpredicted predisposing factor for secondary PTB that is the patients' socio-economic status. It was noted that the incidence rate of secondary PTB significantly higher among operated patients who had been classified at the category of low socio-economic status as compared to other patients who already categorized at high socio-economic class. The income per month was considered as main indicator that had been used for this process of categorization i.e. those patients have been considered as high socio-economic status they got more than 2500LD (~ >1000$) as salary per month, in accordance those who classified as medium socio-economic status they had 1000-2500LD (~400-1000$) as salary per month, and the patients with poor socio-economic status their salary per month was less than 1000LD (~ <400$). The effect of patient's socio-economic status on incidence rate of secondary PTB can be distinguished from the co-existence of limited education levels, poor sanitation conditions as well as bad hygiene circumstances in association with poor socio-economic status. This may affect obviously the post-tonsillectomy care which is the main determinant for post-tonsillectomy nutritional insufficiencies, dehydration, and infection.
Surprisingly there was another factor thought to act as unpredicted predisposing factor for secondary PTB this is the seasonal time of surgery performance. It was confirmed that the incidence rate of secondary PTB higher during summer and autumn seasons as compared to winter and spring seasons. This can be explained by the fact that the risk of postoperative dehydration is significantly increased during summer as well as autumn classes as compared to other two classes this might be due to interaction of two reasons: a) the minimal oral fluids requirements of the patient after tonsillectomy could not be reached because of postoperative odynophagia, and b) the increase of body fluids loss during summer and autumn classes due to excessive sweating as the result of hot climate exposure with insufficient compensation of this loss by needed oral fluids as a sequel of co-existing post-tonsillectomy pain.
On the hand, it was found that the patients who had co-morbid allergic rhinitis were susceptible for secondary PTB as compared to non-allergic patients this should be discussed by the persistence of post-operative mouth breathing as the result of congested nose with or without hypertrophied turbinates as pathognomonic changes of allergic rhinitis. The concomitant mouth breathing will result in uncontrolled oral dryness that predispose for local infection this might be due to two suggested reasons: a) the oral dryness means decrease of secreted saliva volume this resulting in the significant dropping of secretory immunoglobulin (IgA) level that lead to activation of opportunistic oral cavity flora and b) the reduction of saliva secretion might be considered as a significant cause for the disturbance in normal oral cavity alkaline PH this also may contribute to overgrowth of certain strains of normal oral cavity flora or increase the risk of exogenous opportunistic infections.
In accordance, it was elucidated that the patients who had been diagnosed as GERD shown significantly higher risk of secondary PTB as compared to other patients this should be correlated to: a) gastric acidity direct effect: the secondary PTB occurs as the result of local reactive acute inflammatory changes to chemical effect of gastric juice, and b) gastric acidity indirect effect: this mainly due to the significant dropping in the alkaline buffering oropharyngeal PH that lead to the important variation of normal oropharyngeal flora and subsequent infection by the opportunistic microorganisms.
Comprehensively, there was another important factor which had been suggested to be as significant predisposing factor for secondary PTB this is the way of presentation for postoperative instructions by the medical staff and to who these instructions are given. It was noted that if the postoperative instructions are given to the patients as written file rather than verbal description this will reduce significantly the risk of secondary PTB. In accordance if the postoperative instructions are given to patients' mothers or patients themselves among operated children and adult patients consecutively rather than they are given to other patients' relatives as fathers, grandfathers, grandmothers, brothers, sisters, uncles, aunts, or friends this will create a significant improvement in the incidence rate of secondary PTB.
Although among this serial study we tried to highlight the effect of some of suggested unpredicted factors which may play a significant role in determination of incidence rate of secondary PTB but we think that further formative studies are recommended to confirm our results at different media and environments also other possible factors which not studied yet can be thought and postulated.
References
- 1.JP1 Windfuhr, Chen Y S. (2003) Post-tonsillectomy and -adenoidectomy hemorrhage in nonselected patients. Ann Otol Rhinol Laryngol. 112(1), 63-70.
- 2.Windfuhr J P, Chen Y S. (2001) Hemorrhage following pediatric tonsillectomy before puberty. Int J Pediatr Otorhinolaryngol. 58(3), 197-204.
- 3.Windfuhr J P, Chen Y S, Remmert S. (2005) Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients. Otolaryngol Head Neck Surg. 132(2), 281-6.
- 4.Windfuhr J P, Chen Y S. (2002) Incidence of post-tonsillectomy hemorrhage in children and adults: a study of 4,848 patients. Ear Nose Throat J. 81(9), 626-8.
- 5.Myssiorek D, Alvi A. (1996) Post-tonsillectomy hemorrhage: an assessment of risk factors. , Int J Pediatr Otorhinolaryngol 37(1), 35-43.
- 6.Collison P J, Mettler B. (2000) Factors associated with post-tonsillectomy hemorrhage. Ear Nose Throat J. 79(8), 640-2.
- 7.Wei J L, Beatty C W, Gustafson R O. (2000) Evaluation of posttonsillectomy hemorrhage and risk factors. Otolaryngol Head Neck Surg. 123(3), 229-35.
- 8.Roberts C, Jayaramachandran S, Raine C H.A prospective study of factors which may predispose to post-operative tonsillar fossa haemorrhage. Clin Otolaryngol Allied Sci. 17(1), 13-7.
- 9.Attner P, Haraldsson P O, Hemlin C.Hessén Soderman AC. A 4-year consecutive study of post-tonsillectomy haemorrhage. , ORL J Otorhinolaryngol Relat Spec 71(5), 273-8.
- 10.Mutz I, Simon H.Hemorrhagic complications after tonsillectomy and adenoidectomy. Experiences with 7,743 operations in 14 years. , Wien Klin Wochenschr 105(18), 520-2.
- 11.Chowdhury K, Tewfik T L, Schloss M D. (1988) Post-tonsillectomy and adenoidectomy hemorrhage. , J Otolaryngol 17(1), 46-9.
- 12.Arnoldner C, MCh Grasl, Thurnher D, Hamzavi J S, Kaider A et al. (2008) Surgical revision of hemorrhage in 8388 patients after cold-steel adenotonsillectomies. , Wien Klin Wochenschr.120(11-12): 336-42.
- 13.Zielnik-Jurkiewicz B, Rakowska M. (2005) Analysis of postoperative hemorrhage after adenoidectomy and tonsillectomy in children in own material. , Otolaryngol Pol 59(1), 71-6.
- 14.Schrock A, Send T, Heukamp L, Gerstner A O, Bootz F et al. (2009) The role of histology and other risk factors for post-tonsillectomy haemorrhage. Eur Arch Otorhinolaryngol. 266(12), 1983-7.
- 15.Kendrick D, Gibbin K. (1993) An audit of the complications of paediatric tonsillectomy, adenoidectomy and adenotonsillectomy. Clin Otolaryngol Allied Sci. 18(2), 115-7.
- 16.TA1 Tami, Parker G S, Taylor R E. (1987) Post-tonsillectomy bleeding: an evaluation of risk factors. Laryngoscope. 97(11), 1307-11.
- 17.Scheckenbach K, Bier H, Hoffmann T K, Windfuhr J P, Bas M et al. (2008) Risk of hemorrhage after adenoidectomy and tonsillectomy. Value of the preoperative determination of partial thromboplastin time, prothrombin time and platelet count. , HNO 56(3), 312-20.
- 18.Vaiman M, Eviatar E, Shlamkovich N, Segal S. (2003) Effect of modern fibrin glue on bleeding after tonsillectomy and adenoidectomy. Ann Otol Rhinol Laryngol. 112(5), 410-4.
- 19.Randall D A, Hoffer M F. (1998) . , Complications of tonsillectomy and adenoidectomy.Otolaryngol Head and Neck Surg 118, 61-68.
- 20.Clark M P, Waddell A. (2004) The surgical arrest of post-tonsillectomy haemorrhage: hospital episode statistics. , Ann R Coll Surg Engl 86(6), 411-412.
- 21.Krishna P, Lee D. (2001) Post-tonsillectomy bleeding: a meta-analysis. , Laryngoscope 111(8), 1358-1361.
- 22.Peterson J, Losek J D. (2004) Post-tonsillectomy hemorrhage and pediatric emergency care. Clin Pediatr (Phila). 43(5), 445-8.
- 23.Kim D W, Koo J W, Ahn S H, Lee C H, Kim J W. (2010) Difference of delayed post-tonsillectomy bleeding between children and adults. Auris Nasus Larynx. 37(4), 456-60.
- 24.Ahsan F, Rashid H, Eng C. (2004) Is secondary hemorrhage after tonsillectomy in adults an infective condition? Objective measures of infection in a prospective cohort. , Clin Otolaryngol 32(1), 24-7.
- 25.Evans A S, Khan A M, Young D.Assessment of secondary hemorrhage rates fallowing adult tonsillectomy-a telephone survey and literature review. Clin Otolaryngol Allied Sci. 28(6), 489-91.
- 26.Windfuhr J P, Wienke A, Chen Y S. (2009) Electrosurgery as a risk factor for secondary post-tonsillectomy hemorrhage. , Eur Arch Otorhinolaryngol 266, 111-6.
- 27.D'Agostino R, Taro V, Calevo M G.Post-tonsillectomy late hemorrhage: Is it a preferably night-time event?. , Int J Pediatr Otorhinolaryngol 73(5), 713-6.
- 28.Wieland A, Belden L, Cunningham M.Preoperative coagulation screening for adenotonsillectomy: A review and comparison of current physician practices. Otolaryngology–Head and Neck Surgery.2009;140(4):. 542-7.
- 29.Windfuhr J P, Schloendorff G, Baburi D, Kremer B. (2008) Life-threatening posttonsillectomy hemorrhage. , Laryngoscope 118(8), 1389-94.
- 30.Walker P, Gillies D.Post-tonsillectomy hemorrhage rates: Are they technique-dependent?Otolaryngol Head Neck Surg. 2007;136(4 Suppl):S27–31
- 31.Heidemann C H, Wallén M, Aakesson M. (2009) Post-tonsillectomy hemorrhage: assessment of risk factors with special attention to introduction of coblation technique. , Eur Arch Otorhinolaryngol 266(7), 1011-5.
- 32.Bennett A M, Clark A B, Bath A P. (2005) Meta-analysis of the timing of hemorrhage after tonsillectomy: an important factor in determining the safety of performing tonsillectomy as a day case procedure. , Clin Otolaryngol 30(5), 418-23.
- 33.Benson-Mitchell R. (1993) Assessment of sequelae at home following adenotonsillectomy. A basis for day-case management?. , Clin. Otol. Allied Sci 18(4), 282-284.
- 34.Blakley B W. (2009) Post-tonsillectomy bleeding: How much is too much? OtolaryngolHead Neck Surg. 140(3), 288-90.
- 35.Lowe D, Cromwell D A, Lewsey J D. (2009) Diathermy power settings as a risk factor for hemorrhage after tonsillectomy. Otolaryngol Head Neck Surg. 140(1), 23-8.
- 36.Siddiqui R U, Rasheed K, Rafique M. (2004) Tonsillectomy-control of hemorrhage Silk Ligation v/s Bipolar Diathermy. , Pak J Otolaryngol 20(3), 48-50.
