Abstract
Background:
Isoflavones are phytoestrogens present in natural sources, and they resemble estradiol in structure and manner of action. The aim of the study was to assess the effects of soy-milk on serum tHcy levels and to assess the glycemic and lipidemic status of Bangladeshi postmenopausal women.
Methods:
Thirty-six women (aged 50 ±5.16 years, M ±SD) participated in a randomized, un-blinded, open-ended, crossover study design for 52 days. The soy-milk group consumed 350 mL of milk twice a day for 21- day; the milk contained ~30 mg of isoflavones. FBG, PPG, HbA1c, TC, TG, HDL-C, NEFA, and tHcy were measured on day 0, day 21, day 31, and day 52 with a 10- day washout period.
Results:
After the consumption of soy-milk, the level of HDL-C significantly (p=0.005) increased on day 21 in the subjects. No significant changes were observed between the groups. After crossover, significant changes in FBG (p=0.005) and TG (p=0.049) were observed on day 52 in the soy-milk group. Significant improvement in TG (p=0.001) and HDL-C (p=0.032) was also seen at the end-point.
Conclusions:
Soy isoflavones is to some extent favorable to reduce CVD risk factors among Bangladeshi postmenopausal women.
Author Contributions
Academic Editor: Sadanand Naik, HOD (Clinical Biochemistry), K.E.M.Hospital, Pune, India
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2017 Farjana Rahman Bhuiyan, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The Women’s Health Initiative has recently forced practitioners to reconsider their options for the prevention of cardiovascular diseases (CVDs) in postmenopausal women 1. The risk of CVDs increases after menopause, which may be related to substantial metabolic changes that occur as women transit from premenopause to postmenopause. In many women, some features of the metabolic syndrome (abdominal adiposity, insulin resistance, dyslipidemia, and hypertension) emerge with estrogen deficiency. Furthermore, it is also known that concentration of blood homocysteine (Hcy) is an independent risk factor for CVD. Total homocysteine (tHcy) is higher in postmenopausal than that in premenopausal women 2. Although hormonal replacement therapy (HRT) looks to decrease Hcy levels 3, this therapy also increases the risk of CVD and breast cancer 1.
HRT helps improve the quality of life of menopausal women. However, due to its high cost and probable side-effects, alternative therapy is now seriously being sought for. And, isoflavones are now getting attention as an alternate medicine. These are phytoestrogens, i.e. plant compounds, whose phenolic ring is similar to 17β-estradiol and that can bind to the estrogen receptor with a decreased affinity 4. Results of several studies have shown the beneficial effects of isoflavones on the tHcy level 5, 6, although others did not observe any changes 7, 8, 9, 10, 11. In the case of lipid level, some studies reported favorable effect 12, 13. However, a study in Bangladesh revealed that the dietary formononetin, one specific type of phytoestrogens, had no advantageous effect in reducing CVD risks in menopausal women 10.
Although soy-milk is now popular in Bangladesh and it is known that the postmenopausal women of our population do not get enough support due to our poor socioeconomic condition, illiteracy, ignorance, and inadequate healthcare system, and they are at risk of estrogen deficiency.
The consumption of soy products such as soy-milk containing isoflavones might help reduce the risk factors of CVD in menopausal women. The aim of this study was to assess the effects of soy-milk on serum tHcy levels, glycemic and lipidemic status among Bangladeshi postmenopausal women.
Materials and Methods
Subjects
The study was conducted at the Department of Biomedical Research Group (BMRG), BIRDEM, Dhaka, Bangladesh, during March-October 2012. Thirty-six postmenopausal women participated in the study. The study included those who were: aged between > 50 years; postmenopausal without the menstrual cycle for at least the one year; non-user of HRT and had an intact uterus, and also willing to obey the protocol and agreed to sign the written informed consent. The study excluded those who were receiving any oral contraceptives or hormone replacement therapy within the last three months; those who had a menstrual period of <12 months before initiation of the study protocol; those with any chronic illness advised for hospitalization; and those who were unable to answer. The minimum sample-size required was calculated using the formula 14 (μ1- μ2)2= f(α, P)σ2(1/n+1/n); where, μ1- μ2= 1; significance level (α) = 0.05; power (P) = 0.09, which gives f(α, P)=10.5; σ= 1.0.
Study Design
This randomized, un-blinded, open-ended, crossover study lasted for 52 days. During the study period, the patients made four visits (before and after the intervention including the washout period). All the postmenopausal women were randomly divided into two groups: Group A and Group B.
The postmenopausal women of Group A received soy-milk and of Group B received conventional diet for three weeks and after the 10-day washout period, Group B received soy-milk, and group A received conventional diet for another three weeks (Figure 1).
The soy-milk groups consumed 350 mL of soy-milk twice a day; the milk contained ~30 mg of isoflavones. The number of isoflavones was calculated following the instructions of the Japan-Bangladesh Cultural Exchange Association 15. An amount of 350-mL soy-milk was prepared from the 100 g bean following the standard procedure and kept in the refrigerator 15.
On the appointment date, patients visited the Department after overnight (8-12 hours) fasting. Fasting blood samples (5 mL) were drawn from the antecubital vein. The time of drawing blood samples was recorded as 0 minutes. Then the patients received the specific amount of soy-milk for three weeks. Blood parameters (FBG, PPG, HbA1c, TC, TG, HDL-C, NEFA, and tHcy) were measured on day 0 and again on day 21 after taking soy-milk and before and after day 31 and day 52 after the 10-day washout period. During this experiment, the subjects were requested not to take any kind of rich food and isoflavones-rich foods, such as mung, masoor dals, soybean, raw garlic, green bean, potatoes, sweet potatoes, nuts, chickpeas, wheat flour, grapefruit, dates, egg, and nut.
The blood samples were taken in a heparin-containing tube and centrifuged immediately. The serum was separated from the blood samples and stored at -30 0C for biochemical analysis.
Laboratory Analyses
Fasting serum glucose was analyzed using glucose oxidase method (Randox, UK). High-performance liquid chromatography (HPLC) method (Variant II, Bio-Rad Laboratories, Hercules, CA, USA) was used for measuring glycatedhaemoglobin (HbA1c). Serum total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and serum non-esterified fatty acid (NEFA) were measured using enzymatic-colorimetric method (Randox, UK) with an automated analyzer (Hitachi 704, Tokyo, Japan). The LDL-cholesterol in serum was calculated using the Friedwald formula 16. tHcy was measured using fluorescence polarization immunoassay (FPIA) method, with a conventional immuno chemistry auto analyzer (AxSYM system, Abbott diagnostics, USA).
Statistical Analysis
Statistical tests were considered significant at the p value of ≤0.05. Results were expressed as M±SD for descriptive analysis. Paired t-test was performed to determine the effects of soy-milk on the CVD risks among postmenopausal women. And student t-test was performed for group comparison. The SPSS software (Windows version 16.0) was used for the analysis and interpretation of data.
Ethical Aspects
Informed written consent was obtained from all the participants after a full explanation of nature, purpose, and procedures used for the study. Ethical approval was obtained from the ethics and research review committees of the Diabetic Association of Bangladesh.
Results
The mean age of the postmenopausal women was 50 ±5.16 years, and the mean duration of their menopause was 4 ±2.71 years. Of the patients, 94.4% came from the urban area. The mean duration of years of education was 8 ±4 years. Nearly half (41.7%) of the menopausal women had a monthly family expenditure of Taka 5,000-10,000, and 27.4% were home-makers.
The mean body mass index (BMI) was 25.14 ±3.55 kg/m2. Of the menopausal women, 27.78% were at increased risk of overweight, and 44.44% were at the acceptable range of BMI 17.
Table 1 shows the baseline characteristics of the postmenopausal women.
Table 1. Baseline characteristics of postmenopausal women (n=36)| Variables | |
| Body mass index (kg/m2) | 25.14 ±3.55 |
| Underweight | 2 (5.6%) |
| Increasing but acceptable risk | 8 (22.2%) |
| Increased risk | 18 (50%) |
| High risk | 8 (22.2%) |
| Systolic blood pressure (mmHg) | 114±11.61 |
| Diastolic blood pressure (mmHg) | 75±10.03 |
| Fasting blood glucose (mmol/L) | 5.37±0.68 |
| Postprandial glucose (mmol/L) | 6.42±1.02 |
| HbA1c (%) | 5.92±0.61 |
| S Triglyceride (mg/dL) | 159.92±63.83 |
| S Cholesterol (mg/dL) | 215.03±44.55 |
| S HDL-C (mg/dL) | 41.97±8.08 |
| S LDL-C (mg/dL) | 140.56±36.97 |
| NEFA (mmol/L) | 0.34 ±0.19 |
| S tHcy (µmol/L) | 10.40±4.60 |
The effects of soy-milk on glycemic, lipidemic and tHcy levels of the postmenopausal women are shown in Table 2. No significant changes were found in tHcy, fasting blood glucose (FBG), serum triglycerides (TG), serum total cholesterol (TC), and serum LDL-C between and within the groups except on serum HDL-C. In the soy-milk group, the level of serum HDL-C significantly increased (45.22 ±6.20 vs 39.00 ±7.30, p= 0.005) after the consumption of soy-milk, although between the groups no significant changes were observed.
Table 2. Effect of soy-milk on glycemic, lipidemic, and tHcy level among postmenopausal women| Variable | Day 0 (n= 36) | Day 21 (n= 36) | p value |
| tHcy (mg/S) | |||
| Control roup (n=18) | 11.81±5.93 | 11.67±7.19 | 0.791 |
| Soy-milk group (n=18) | 8.98±2.05 | 8.93±1.86 | 0.89 |
| p value | 1.91/0.065 | 1.57/0.127 | |
| FBG (mmol/L) | |||
| Control group (n=18) | 5.28±0.65 | 5.39±0.69 | 0.467 |
| Soy-milk group (n=18) | 5.46±0.72 | 5.33±0.57 | 0.369 |
| p value | 0.442 | 0.774 | |
| S TG (mg/dL) | |||
| Control group (n=18) | 160.11±65.89 | 152.28±28.35 | 0.602 |
| Soy-milk roup (n=18) | 159.72±63.62 | 133.72±23.36 | 0.088 |
| p value | 0.986 | 0.039 | |
| S TC (mg/dL) | |||
| Control roup (n=18) | 212.44±42.15 | 210.67±41.2 | 0.777 |
| Soy-milk group (n=18) | 217.61±47.91 | 220.17±50.89 | 0.803 |
| p value | 0.733 | 0.542 | |
| S HDL-C (mg/dL) | |||
| Control group (n=18) | 44.94±7.90 | 46.00±6.24 | 0.461 |
| Soy-milk group (n=18) | 39.00±7.30 | 45.22±6.20 | 0.005 |
| p value | 0.025 | 0.633 | |
| S LDL-C (mg/dL) | |||
| Control group (n=18) | 135.56±33.76 | 131.28±32.76 | 0.554 |
| Soy-milk group (n=18) | 145.56±40.26 | 151.11±44.46 | 0.419 |
| p value | 0.425 | 0.137 |
After crossover, significant changes were observed in FBG (5.18 ±0.49 vs 5.56 ±0.43, p=0.005) and TG (138.33 ±53.03 vs 180.61 ±98.93, p=0.049) in the soy-milk group. No significant changes were observed in other parameters within or between the groups (Table 3).
Table 3. Effect of soy-milk on glycemic, lipidemic and tHcy level among postmenopausal women| Variable | Day 31 (n= 36) | Day 51 (n= 36) | p value |
| tHcy (mg/S) | |||
| Control group (n=18) | 8.32 ±1.89 | 8.37 ±1.92 | 0.882 |
| Soy-milk group (n=18) | 10.96 ±5.33 | 10.94 ±5.68 | 0.963 |
| p value | 0.056 | 0.078 | |
| FBG (mmol/L) | |||
| Control group (n=18) | 5.39 ±0.51 | 5.23 ±0.49 | 0.338 |
| Soy-milk group (n=18) | 5.56 ±0.43 | 5.18 ±0.49 | 0.005 |
| p value | 0.297 | 0.761 | |
| S TG (mg/dL) | |||
| Control group (n=18) | 149.67 ±45.23 | 122.22 ±39.40 | 0.011 |
| Soy-milk group (n=18) | 180.61 ±98.93 | 138.33 ±53.03 | 0.049 |
| p value | 0.236 | 0.308 | |
| S TC (mg/dL) | |||
| Control group (n=18) | 207.56 ±40.62 | 215.17 ±39.01 | 0.219 |
| Soy-milk group (n=18) | 212.22 ±34.15 | 208.11 ±43.91 | 0.507 |
| P value | 0.711 | 0.614 | |
| S HDL-C (mg/dL) | |||
| Control group (n=18) | 42.78 ±5.81 | 41.06 ±6.51 | 0.333 |
| Soy-milk group (n=18) | 39.50 ±3.18 | 43.29 ±12.54 | 0.195 |
| p value | 0.043 | 0.506 | |
| S LDL-C (mg/dL) | |||
| Control group (n=18) | 134.72 ±39.57 | 143.17 ±33.21 | 0.102 |
| Soy-milk roup (n=18) | 131.22 ±35.31 | 134.44 ±33.45 | 0.672 |
| p value | 0.781 | 0.438 |
Levels of tHcy, FBG, serum TG, serum TC, serum HDL-C, and serum LDL-C were estimated for each patient at the beginning of the study and at the end of 52 days. A significant improvement was seen in serum TG (136.64 ±38.55 vs 162.53 ±70.50, p=0.001) and HDL-C (43.84 ±8.36 vs 41.56 ±6.65, p=0.032) levels in patients taking soy-milk, and tHcy and FBG levels were found to improve but not significantly. Serum TC and LDL-C showed no changes (Table 4).
Table 4. Changes of total homocysteine, glycemic & lipidemic status at baseline and after day 51 of intervention in postmenopausal women (n=36)| Variable | Baseline | End-point | p value |
| tHcy (mg/dL) | 10.02 ±4.37 | 9.98 ±4.87 | 0.840 |
| FBG (mmol/L) | 5.43 ±0.59 | 5.29 ±0.56 | 0.061 |
| S TG (mg/dL) | 162.53 ±70.50 | 136.64 ±38.55 | 0.001 |
| S TC (mg/dL) | 212.46 ±40.77 | 213.53 ±43.30 | 0.768 |
| S HDL-C (mg/dL) | 41.56 ±6.65 | 43.84 ±8.36 | 0.032 |
| S LDL-C (mg/dL) | 136.76 ±36.92 | 140.00 ±36.37 | 0.328 |
Figure 2 shows the changes in serum NEFA between the baseline (0.34±0.20) and the endpoint (0.27 ±0.17). These changes were insignificant.
Figure 2.Changes in NEFA level at baseline and endpoint (n=36)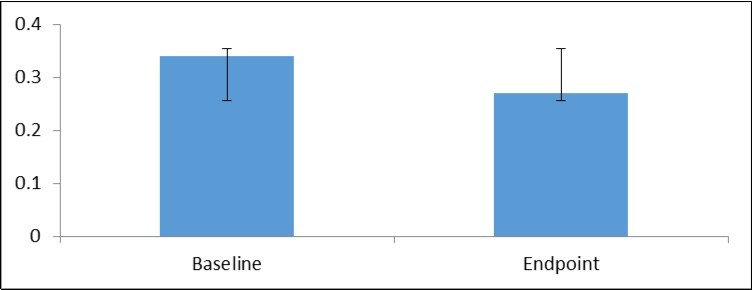
Discussion
The results of the present study indicate that ~30-mg dietary isoflavones had little effect on CVD risk markers, such as Hcy, TG, TC, and HDL-C in the healthy postmenopausal women. In the present study, the intake of soy-milk by the postmenopausal women slightly altered the level of tHcy but not significantly. This result coincides with results of some double-blind, placebo-controlled, randomized, crossover intervention studies 7, 8 where 50-100 mg of dietary isoflavones did not show any effect on tHcy in the healthy postmenopausal women. Results of another study revealed that isoflavones did not protect against CVD risk factors whereas soy-protein with native phytate significantly reduced tHcy and iron stores in menopausal women 9. No significant association was found between phytoestrogen intake and serum tHcy level in a study among Bangladeshi healthy postmenopausal women 10. However, the present findings contradicted results of a study by Tonstad et al. 5 who reported that soy-protein with isoflavones had a tHcy-lowering effect. The same results were found in a study among Turkish postmenopausal women where standardized isoflavones were used instead of isolated soy-protein 6.
In the present study, after the consumption of soy-milk, level of triglycerides significantly (p≤0.05) reduced, and level of HDL-C significantly (p≤ 0.05) improved in the postmenopausal women, although other parameters, such as total cholesterol, NEFA, and fasting blood glucose, showed a little change; however, LDL-C did not show any progress. It was initially thought that phytoestrogen or its subgroup isoflavones present in food could account for the lipid benefits 12, 13, 18, 19.This concept was challenged by data that showed no significant effect of isoflavones on circulating lipid concentrations 20, 21, 22, and even no association was found between isoflavones and lipid level in postmenopausal women 10. The results of the present study more or less coincided with results of these studies.
No data on the effects of isoflavones on NEFA are available, which is also the important marker for CVDs. In the present study, serum concentrations of NEFA marginally reduced during the isoflavones regimen but not significantly. This finding indicates that isoflavones may help alter the NEFA level.
The detection of the physiologic effects of dietary soy is a complicated matter because soy-protein contains many components, such as isoflavones, phytate, saponins, and β-conglycinin, each of which may be responsible for the beneficial effect. Differing results between the present study and others may be influenced due to the absence of extraction of isoflavones in soy-milk, failed to quantify individual isoflavones amount, calculated total isoflavones using literature value 15, and the shortage period of intervention. However, the present study also had a couple of limitations, such as study design, short duration of intervention, and usages of literature-based value. Beside these, it could not possible to collect any concrete evidence against their dietary practice during experimental time due to the shortage of manpower and funds.
Conclusions
In the present study, soy isoflavones are to some extent favorable for reducing CVD risks though isoflavones did not act as a protector against CVD risk factors in the postmenopausal women. A careful study design is necessary to clearly elucidate the effects of soy isoflavones. If the prolonged usages of the regimen can be run, there is a possibility of the advantageous effect of soy-milk on CVD risks among Bangladeshi postmenopausal women.
Authors’ Contributions
FRB: contributed her intellectual ability to conception and design of the research, analysis and interpretation of data; drafting the article, revising it critically for important intellectual content, and final approval of the version to be published. FS: contributed her intellectual ability to conception and design of the research; drafting the article, revising it critically for important intellectual content, and final approval of the version to be published. IRH: contributed her intellectual skill in analysis and interpretation of data. KJ: contributed her intellectual skill in the revision of the manuscript. LA: Revision of manuscript for important intellectual content. All of the above authors read and approved the final manuscript.
Acknowledgments
We highly acknowledge our respected colleague Mr. M. Shamsul Islam Khan, Advisor, Department of Library and In-Charge, English Foundation Course, Department of Applied Languages and Culture, Bangladesh University of Health Sciences, for his guidance in language editing. We thank the postmenopausal women who participated in the study.
References
- 1.Rossouw J E, Anderson G L, Prentice R L, LaCroix A Z, Kooperberg C et al. (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. , Jama; 288(3), 321-33.
- 2.Hak A E, Polderman K H, Westendorp I C, Jakobs C, Hofman A et al. (2002) Increased plasma homocysteine after menopause. , Atherosclerosis; 149(1), 163-8.
- 3.Madsen J S, Kristensen S R, Klitgaard N A, Bladbjerg E M, Abrahamsen B et al. (2002) Effect of long-term hormone replacement therapy on plasma homocysteine in postmenopausal women: a randomized controlled study. American journal of obstetrics and gynecology;. 187(1), 33-9.
- 4.Kuiper G G, Carlsson B, Grandien K, Enmark E, Haggblad J et al. (1997) Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. , Endocrinology; 138(3), 863-70.
- 5.Tonstad S, Smerud K, Hoie L. (2002) A comparison of the effects of 2 doses of soy protein or casein on serum lipids, serum lipoproteins, and plasma total homocysteine in hypercholesterolemic subjects. The American journal of clinical nutrition;. 76(1), 78-84.
- 6.Turhan N O, Duvan C I, Bolkan F, Onaran Y. (2009) Effect of isoflavone on plasma nitrite/nitrate, homocysteine, and lipid levels in Turkish women in the early postmenopausal period: a randomized controlled trial. , Turkish Journal of Medical Sciences; 39(3), 367-75.
- 7.Reimann M, Dierkes J, Carlsohn A, Talbot D, Ferrari M et al. (2006) Consumption of soy isoflavones does not affect plasma total homocysteine or asymmetric dimethylarginine concentrations in healthy postmenopausal women. , The Journal of nutrition; 136(1), 100-5.
- 8.Brandao L C, Hachul H, Bittencourt L R, Baracat E C, Tufik S et al. (2009) Effects of isoflavone on oxidative stress parameters and homocysteine in postmenopausal women complaining of insomnia. , Biological research; 42(3), 281-7.
- 9.Hanson L N, Engelman H M, Alekel D L, Schalinske K L, Kohut M L et al. (2006) Effects of soy isoflavones and phytate on homocysteine, C-reactive protein, and iron status in postmenopausal women. The American journal of clinical nutrition;. 84(4), 774-80.
- 10.Saleh F, Afnan F, Ara F, Yasmin S, Nahar K et al. (2011) Phytoestrogen intake and cardiovascular risk markers in Bangladeshi postmenopausal women. Mymensingh medical journal : MMJ;. 20(2), 219-25.
- 11.Song X, Zeng R, Ni L, Liu C. (2016) The effect of soy or isoflavones on homocysteine levels: a meta‐analysis of randomised controlled trials. , Journal of Human Nutrition and Dietetics; 29(6), 797-804.
- 12.Bairey Merz CN, Johnson B D, Braunstein G D, Pepine C J, Reis S E et al. (2006) Phytoestrogens and lipoproteins in women. The Journal of clinical endocrinology and metabolism;. 91(6), 2209-13.
- 13.Allen Jerilyn K, Becker Diane M, Kwiterovich Peter O, Lindenstruth Kathleen A, CCB S. (2007) Effect of soy protein-containing isoflavones on lipoproteins in postmenopausal women. , Menopause; 14(1), 106-14.
- 16.Friedewald W T, Levy R I, Fredrickson D S. (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry;. 18(6), 499-502.
- 17. (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London. , England); 363(9403), 157-63.
- 18.Jassi H K, Jain A, Arora S, Chitra R. (2010) Effect of soy proteins Vs soy isoflavones on lipid profile in postmenopausal women. Indian journal of clinical biochemistry:. , IJCB; 25(2), 201-7.
- 19.Rebholz C M, Reynolds K, Wofford M R, Chen J, Kelly T N et al. (2013) Effect of soybean protein on novel cardiovascular disease risk factors: a randomized controlled trial. European journal of clinical nutrition;. 67(1), 58-63.
- 20.Simons L A, M von Konigsmark, Simons J, Celermajer D S. (2000) Phytoestrogens do not influence lipoprotein levels or endothelial function in healthy, postmenopausal women. The American journal of cardiology;. 85(11), 1297-301.

