Abstract
Objective
To evaluate the effect of a single intraarticular dose of Gonyautoxins for pain control after Total Knee Arthroplasty (TKA).
Subjects
30 consecutive patients with osteoarthritis with Kellgren & Lawrence level of two or more, who required TKA, were enrolled.
Methods
Subjects receive a single intra-articular infiltration of 40 µg dose of Gonyautoxins, immediately after TKA wound closure. The pain was measured with the Visual Analog Scale (VAS). Additionally, the range of motion at 12, 36, and 60 hours and hospital stay length were recorded. Results were compared to the 2014 TKA cohort.
Results
25 patients (83.33%) achieved successful pain management. All patients achieved complete flexion ≥90° 60 hours after surgery and 24 patients achieved full extension before hospital discharge. The median VAS pain score for each evaluation period was ≥2. The 25 Gonyautoxins treated patients who achieved successful pain management had a median VAS pain score of 0 after 36 and 60 hours.
Conclusions
Gonyautoxins are safe and effective in pain management after TKA when used as a single intra-articular dose. This protocol shows adequate pain control in TKA, reducing discharge to 3 days and greater range of motion, improving the post-operated patient experience.
Author Contributions
Academic Editor: Amal Ibrahim Hassan Ibrahim, Department of radioactive isotopes, Egypt
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2018 Jaime Hinzpeter, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The articular replacement has become the surgery of the 20th century, with excellent results in total hip arthroplasty. Total knee arthroplasty (TKA), however, has not seen similar results, as only 85% of patients are satisfied post-surgery 1, 2, 3, 4, and the remaining 15% complain of acute and chronic pain 5, 6. Correct pain management in TKA can eliminate severe pain and reduce the length of inpatient stay, opioid use, costs, and incidence of chronic pain 7, 8, 9, 10, 11, 12, 13.
Pain management is crucial after TKA since post-operative pain is the most important issue for patients 5, 6. Pain after TKA is associated with venous thromboembolism, coronary ischemia, pneumonia, insomnia, delirium, paralytic ileus, complex regional pain syndrome, urinary retention, arthrofibrosis, and delay in rehabilitation. Prolonged postoperative severe pain is the best predictor of chronic pain 7, 8, 9, 14, 15.
On the other hand, actual pain control protocols interfere with rehabilitation and produce unwanted side effects 16. For example, continuous epidural infusion and significant nerve blockage are associated with paresis that can delay rehabilitation, increase hospital stay, and increase the risk of falls, which can add other complications. Therefore, a delicate balance is required between the provision of adequate pain relief and early mobilisation. For its part, intravenous patient-controlled analgesia is associated with nausea, vomiting and delirium in elderly patients 17. All of the aforementioned are reasons why the local treatment of pain has become a better option for pain relief.
The literature describes several options for local pain treatment after TKA 16, using a single or a combination of local anaesthetics, NSAIDs, corticosteroids, morphine, antibiotics, and epinephrine; however, these options can only achieve close to 48 hours of pain relief 7, 9, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27. Both, intra and extra-articular local infiltrations have been reported to have comparable efficacy in reducing pain 28. Thus, controversy remains regarding the optimal post-operative analgesic regimen following TKA.
Gonyautoxins are phycotoxins that belong to the group of Paralytic Shellfish Poison (PSP], they are non-protein phycotoxins of low molecular weight, which are soluble in water, and structurally related to Saxitoxin. The PSP toxins are responsible for the human syndrome known as Paralytic Shellfish Poisoning caused by the consumption of mollusc that feeds on toxic dinoflagellates [29,30,31].The effects of Gonyautoxins are associated to their reversible, highly-selective blockage of the outer pore of voltage-gated sodium channels in neurons, inhibiting channel opening and therefore blocking neuronal transmission at the axonal and neuromuscular junction levels. Consequently, Gonyautoxins prevent the propagation of action potentials and interrupt neuronal communication, producing anaesthesia and flaccid paralysis of the innerved zone 32,33,34,35,36,37,38. The local infiltration of Gonyautoxins has been shown to be safe and effective in numerous clinical applications 39. In a recent publication, our group showed that peri-articular infiltration with Gonyautoxins was safe and effective in postoperative pain control in TKA, reducing hospital stay and opioid consumption. The present study evaluates the effect of a single intra-articular infiltration of Gonyautoxins to manage postoperative pain, to improve the range of movement and rehabilitation after TKA, to reduce hospital stay, and to abolish opioid use. This study is the first testing of Paralytic Shellfish Poison toxins applied in an intra-articular infiltration procedure to control the TKA post-surgery pain.
The main aim of this study is to develop the simplest pain management protocol in TKA to lead to better patient welfare.
Methods
This study was approved by the Ethics Committee of the Chile University Clinical Hospital (Record Nº 70 2015HCUCH). The principles of the International Ethical Guidelines for Biomedical Research Involving Human Subjects and Declaration of Helsinki 40 were followed in the design of the study. Written informed consent was obtained from all patients before enrollment in this study. Thirty patients were recruited between October 2015 and June 2016 from the Department of Orthopedic Surgery, Chile University Clinical Hospital.
Inclusion Criteria
We included 30 consecutive patients who required a unilateral TKA due to osteoarthritis with Kellgren and Lawrence level of two or more, which did not respond to conservative therapy.
Exclusion Criteria.
Patients with psychiatric or neurologic conditions that compromised their comprehension of the study and follow-up, a known seafood allergy, narcotic dependence, or those who rejected the procedure were excluded. A patient who had hepatic transplantation was also excluded. Body mass index, inflammatory osteoarthritis, and severe perioperative deformity were not exclusion criteria.
Surgery Procedure
All patients received a single dose of intradural anaesthetic consisting of 2.5cc of 0.5 % bupivacaine, and a single intravenous bolus of antibiotic prophylaxis (2 g cefazolin) applied 30 minutes before the surgery. Standard TKA was performed with an anterior knee incision and a medial parapatellar approach; use of a tourniquet only during cementation, and no wound drainage. The prosthesis model used in all patients was Knee Vanguard CR AS (BIOMET®). All participants were operated on by two senior surgeons (JH and CB) during 2015 and 2016 at our institution (Chile University Clinical Hospital).
Immediately after wound closure, patients received a single intra-articular injection of 40 µg of Gonyautoxins, diluted in 60 mL of 0.9%saline solutions. The Gonyautoxins purification has been described previously. Briefly, the Gonyautoxins were purified from Paralytic Shellfish Poison highly contaminated shellfish that was collected in the fjords around the Magellan Strait close to Punta Arenas city in the southernmost part of Chile 32, 33, 34, 35, 36, 37, 38. High-performance liquid chromatography determined the toxin purity (98 %) with online fluorescence detection and online mass spectroscopy analysis 32, 33, 34, 35, 36, 37, 38. The Gonyautoxin was diluted in 0.9% saline solution; no other additives were used. The doses were produced at the University of Chile, Faculty of Medicine and Membrane Biochemistry Laboratory with the approval of National Institute of Health, Santiago, Chile.
Postoperatively, all patients received an oral dose of 1000 mg of acetaminophen and 100 mg of intravenous ketoprofen every 8 hours until hospital discharge. For rescue analgesia, 100 mg of tramadol in 100 mL of saline solution was used every 8 hours, at maximum. If a patient refers a VAS > 5, a femoral nerve blockage rescue was indicated, and Gonyautoxins pain control was considered a failure. Thromboprophylaxis 5000 U of subcutaneous dalteparin every 24 hours was administered beginning 12 hours after surgery. Compression stockings were used with all patients. Patients also received standard nursing care, ice packs and wound management. Rehabilitation began the day of the surgery (6 hours after), with in-bed mobilisation. One day post-surgery, patients stood and walked with two canes, with partial weight bearing, and they also had the range of motion (ROM) knee exercises three times per day until discharge. Discharge criteria included the achievement of ROM, the ability to walk alone without canes, and a VAS pain score of less than 5.
Variables
Pre-operatively, all patients’ ROM was measured with an analogue goniometer, and the VAS, The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Oxford Knee Score (OKS) scales were also collected.
At 12, 36, and 60 hours post-surgery, all patients had ROM and VAS pain measurements. The VAS pain score measurement was made, on a scale from 0 to 10, being 0 no pain and 10 maximum pain, a score of 4 or less was considered as successful. During the same assessment periods, ROM was also evaluated with analogue goniometry. A successful ROM outcome was defined as patients achieving full extension (extension = 0°) and full flexion (defined as flexion of 90° or higher). The use of rescue analgesia, clinical complications and duration of hospital stay were recorded for each participant.
TKA Patient’s Cohort: Data Obtained During 2014
To compare the clinical results of this study's patients, we reviewed the clinical records of 81 patients who underwent TKA in 2014 in the same hospital. All 2014 TKA patients received combined spinal anaesthesia, consisting of an injection of fentanyl, epinephrine, bupivacaine, and an epidural of a continuous solution of bupivacaine and fentanyl. The same post-surgery pain management protocol followed in our study was used in the 2014 Cohort. From the starting eighty-one 2014 TKA patients, 12 were excluded from the comparative analysis (6 for having unicompartmental knee arthroplasty, 3 for TKA revisions, one due to a tumour, and two bilateral TKAs performed in one stage), leaving in total 69 patients. Data on VAS pain and hospital length stay were recorded from all 69 patients.
Only 62 had they range of motion recorded.
Statistical Analysis
For continuous variables in which normal distribution could not be assumed, median, range, and interquartile ranges (IQ) are shown, while continuous variables with a normal distribution were summarised with mean and standard deviation. If p-value was higher than 0.15 in Shapiro-Wilks test, a normal distribution was assumed.
Statistical inference was performed by comparing the patients infiltrated with Gonyautoxin against the 2014 TKA patient cohort. Since the Gonyautoxin group consisted of twenty-five patients, the Fisher two-sided test was implemented to compare categorical variables: sex, extension success (= 0°), flexion success (≥90°) and pain success (VAS ≤4).
The binomial distribution was assumed for success in full extension, flexion and VAS pain, then a fitted repeated measurement logistic regression was estimated. Probabilities of one event per patient and odds ratios (OR) were calculated.
A significance level of 0.05 was established, and the 95% confidence intervals were reported. All analyses were performed using Stata v11.2 (StataCorp LP, College Station, Texas, USA).
Results
The 30 patients’ average age was 66 ± 6.6 years. Before surgery, WOMAC and OKS median values were 43 (2.3-75.8, IQ 34.1-54) and 19 (5-29, IQ 17-21), respectively (Table 1).
Table 1. Summary of Patients, age, knee laterality, ROM and Pain VAS at 12, 36, and 60 hours post-surgery, by the Gonyautoxin group and 2014 TKA patient cohort. The right column shows the significance of each test applied.| Variable | Gonyautoxin (+) | 2014 TKA cohort | p-value (test) |
|---|---|---|---|
| n | 25 | 69 | |
| Age | 66 (±6.77) | 66.57 (±8.79) | 0.93 8 (Wilcoxon) |
| Right Knee | 15 (60%) | 35 (51.47%) | 0.31 (Fisher) |
| Male | 13 (52%) | 26 (37.68%) | 0.15 (Fisher) |
| Hospital Stay | 3 (3-5) (IQ 3-3) | 5 (4-20) (IQ 5-6) | 0.00 (Wilcoxon) |
| ROM 12 hrs | 85 (40-100) (IQ75-90) | 90 (40-110) (IQ 90-95) | 0.00 (Wilcoxon) |
| ROM 36 hrs | 90 (70-110) (IQ 90-90) | 90 (60-110) (IQ 90-95) | 0.34 (Wilcoxon) |
| ROM 60 hrs | 100 (85-110) (IQ 90-100) | 90 (80-105) (IQ 90-90) | 0.00 (Wilcoxon) |
| Ext = 0° 12 hrs | 21 (84%) | 25 (39.06%) | 0.00 (Fisher) |
| Ext = 0° 36 hrs | 24 (96%) | 44 (70.97%) | 0.01 (Fisher) |
| Ext = 0° 60 hrs | 24 (96%) | 54 (90.00%) | 0.33 (Fisher) |
| Flex ≥90° 12hrs | 14 (66%) | 43 (67.19%) | 0.22 (Fisher) |
| Flex ≥90° 36hrs | 20 (80%) | 51 (82.26%) | 0.51 (Fisher) |
| Flex ≥90° 60hrs | 25 (100%) | 52 (86.67%) | 0.05 (Fisher) |
| vas pain 12 hrs | 2 (0-6) (IQ 0-2) | 3 (0-8) (IQ 2-5) | 0.00 (Wilcoxon) |
| vas pain 36 hrs | 0 (0–4) (IQ 0-2) | 2 (0–10) (IQ 0-4) | 0.00 (Wilcoxon) |
| vas pain 60 hrs | 0 (0-3) (IQ 0-2) | 1 (0-10) (IQ 0-4) | 0.05 (Wilcoxon) |
| vas ≤ 4 12 hrs | 23 (92%) | 47 (68.12%) | 0.01 (Fisher) |
| vas ≤ 4 36 hrs | 25 (100%) | 54 (78.26%) | 0.01 (Fisher) |
| vas ≤ 4 60 hrs | 25 (100%) | 52 (75.36%) | 0.00 (Fisher) |
Gonyautoxins Success and Clinical Complications
From 30 participating patients, only 5 (16.67%) reported dissatisfaction with the post-surgery pain management and required a rescue femoral nerve block; this outcome was considered a failure of pain control. The remaining 25 patients (83.33%) were satisfied with the Gonyautoxins pain control. No patients had significant complications, although two patients reported a metallic taste sensation on their tongue, which lasted less than 3 hours.
Range of Motion (ROM)
The range of motion 12 hours after surgery was 85° or higher in the 25 patients who responded to Gonyautoxins (Figure 1 and Table 1). The twenty-five patients achieved full flexion 60 hours after surgery. Also, an extension of 0º was achieved by 24/25 Gonyautoxin infiltrated (96%) at 60hours follow up (Table 1).
Figure 1.ROM distribution at 12, 36 and 60 hours post-surgery with Graph boxes. On the Y-axis, the range of motion (ROM) is shown, with 0° at full extension. The upper box shows percentile 75 (Q3), the bottom of the box is percentile 25 (Q1) and the middle line of the box is the median (percentile 50 or Q2). Gray dots represent outliers. The upper limit is calculated by 1.25*(Q3, and inferior is calculated by 1.25*(Q3.
Comparing these data with the one collected from the 2014 TKA patient cohort, the Gonyautoxin-treated patients reached a higher rate of extension success at 12, 36 and 60 hours. Also, 100 % of Gonyautoxin infiltrated reached full flexion after 60 hours, instead of the 2014 TKA Cohort only got 86.67 %. The major difference between both groups was observed in the full extension, where at all times, higher percentages were achieved by the group treated with Gonyautoxins; been the maximum difference quantified at 12 hours after surgery when Gonyautoxin treated group reached 84% of success and the 2014 TKA cohort only 39.06 %. Also, the ROM at 60 hours post-surgery was significantly higher in patients infiltrated with Gonyautoxin who´s accomplished a median ROM of 100°, instead of a median of 90° in the 2014 TKA cohort (Table 1).
Pain
Concerning pain, 12hours post-surgery, the median VAS score for the patients treated with Gonyautoxin was 2, and 23 patients (92%) achieved a VAS score ≤ 4. Instead, the 2014 TKA cohort extended only to 68.12 %. Nevertheless, the other two patients (8%) infiltrated with Gonyautoxin required one bolus of tramadol, afterwards this reinforced treatment to control pain, they achieved a VAS score of 3. Remarkable, 100 % of the patients treated with Gonyautoxin evaluate their pain with the median VAS score of 0 after 36 and 60 hours post-surgery. In contrast, the 2014 TKA cohort showed VAS score ≤ 4 of 68.12, 78.26 and 75.36 % at 12, 36 and 60 hours after surgery respectively (Table 1).
Length of Hospital Stay
The 25 patients (83.33%) who respond to Gonyautoxins protocol had a median hospital stay of 3 days 3, 4, 5, while the five patients that required a femoral nerve blockage had a median hospital stay of 4 days 4. Moreover, the 2014 TKA cohort showed a median of five days length of stay 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20. The Gonyautoxin infiltrated group showed a significantly shorter length of hospital stay than the 2014 TKA patient cohort. (Table 1, Figure 3).
Figure 3.Hospital stay length in Gonyautoxin responders and patients that required a femoral nerve blockage. The dot in Gonyautoxin group represent the 3 patients that had a hospital stay of 5 days, all of them for social reasons.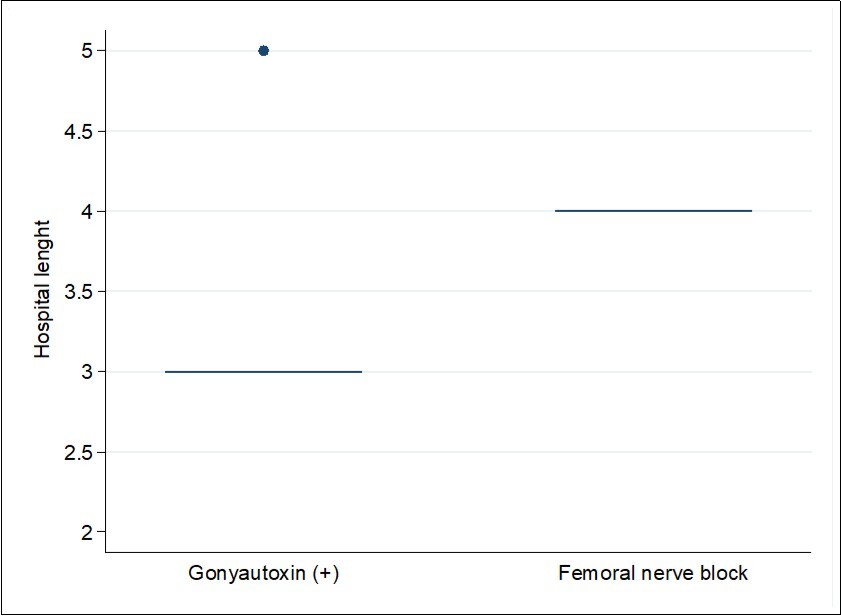
Discussion
Pain management is a hot topic in joint replacement surgery, especially for TKA. This work is our second experience in the use of Gonyautoxins after TKA to achieve satisfactory pain control for patients, reducing the length of hospital stays and improving range of motion.
In a recent article, we demonstrated that Gonyautoxins was successful in pain management after TKA. In it article, Gonyautoxin was applied periarticular in posterior capsule, both retinaculum, both collateral ligaments, quadriceps tendon and patellar tendon, and subcutaneous. Each injection had one cc, for a total dosage of 30cc as peri-articular infiltration procedure in TKA 41. The total dosage used was 40 µg of Gonyautoxin in 30cc, like the present study.
The difference is that this time the doses was a single intraarticular administration after wound closure. The aim was to develop a less complicated procedure.
The new intra-articular infiltration procedure showed to be useful, since over 83% of the patients did not require a rescue femoral nerve block. Furthermore, only two of these patients had a VAS score of 4 or higher, and they received opioid analgesic reinforcement. Nevertheless, 36 hours post-surgery, these two patients did not require additional opiates for pain management.
The most significant finding is that 25 patients achieved full flexion at 60 hours after surgery, and that total extension was achieved by 24 patients (96%). Moreover, after 36 and 60 hours, the median VAS score was 0, and all 25 patients achieved a VAS score equal or less than 4. No tramadol was used with these 25 patients (Table 1 and Figure 2). The 2014 Cohort showed a higher VAS Pain score at 12, 36 and 60 hours and only 75 % of patients showed a VAS ≤ 4 (Table 1), showing that the Gonyautoxin treatment plays a better role in pain control.
Figure 2.Pain VAS score distribution at 12, 36, and 60 hours after surgery.
Also, our second outcome was also accomplished, since the 25 patients who responded to Gonyautoxins pain control (83.33%) had a median hospital stay of 3 days (Figure 3), similar to the 30 points of peri-articular infiltration procedure reported 41. Meanwhile, the five patients who required a femoral nerve blockage had a median hospital stay of 4 days 4. Alongside, the 2014 Cohort average of hospital stay was five days (Table 1 and Figure 3).
It is well known that Gonyautoxins, as all PSP toxins, exerts its effect by reversibly binding to a receptor on voltage-gated sodium channel (NaV channels) on excitable cells, thereby blocking neuronal transmission 32, 33. Nine types of NaV channels have been described, three of which, NaV 1.7, NaV 1.8 and NaV 1.9, are predominantly expressed in peripheral damage-sensing neurons and play a crucial role in inflammatory pain. These channels are highly expressed in dorsal root ganglia of knee joint afferent nerves and increase their expression in response to chronic inflammatory stimulation in knee joints 42, 43, these phycotoxins can also block them.
This new infiltration procedure had a low, but observable failure rate, with 16.67% of patients requiring femoral nerve blockage. In contrast, the patients who received the peri-articular application of the Gonyautoxin in our previous study did not require this femoral block rescue.
As we proposed in our first manuscript 32, 33, 34, 35, 36, 37, 38, the Gonyautoxins infiltrations in several locations would ensure the overall presence of the drug and the significant better anaesthetic effect of the toxin in all points that could cause pain. Maybe, the pain control may depend on the uniformity of the intra-articular drug distribution; the Gonyautoxin should be evenly distributed to reach and block every peri-articular structure. Therefore, blocking all the local transmission points of axonal pain associated conduction.
Nonetheless, the single intra-articular application performed in this study also showed to be safe and effective, but simpler and less invasive than the 30 points peri-articular application. Proposing, that one intra-articular infiltration should be used as pain rescue instead of femoral block.
On the other hand, once more is demonstrated that Gonyautoxins are an excellent option for control pain, blocking the local transmission and axonal conduction when is administrated as one intra-articular dose in the post-surgery period of TKA. The data showed here, using the Gonyautoxin infiltration, highlights the patient welfares of this new protocol of pain control. The one dose of intra-articular infiltration with Gonyautoxin permit early rehabilitation, faster and more significant pain relief, and outstanding ROM.
Conclusions
Gonyautoxins are safe and effective in pain management after TKA when administrated via intra-articular infiltration. For the first time, the effect of blocking pain neuronal transmission by a single intra-articular dose is shown. Results showed that 83.3 % of patients experienced pain relief. This innovative uncomplicated procedure also increased patient´s ROM, reduced VAS pain and the duration of hospital stay. Finally, the pain control is total, and the associated beneficial effects are maintained at least 60 hours in responder patients.
Acknowledgements
This study was supported by the FONDECYT Grant 1130037, sponsored by the Chilean Government.
References
- 1.Bonnin M P, Basiglini L, Archbold H A. (2011) What are the factors of residual pain after uncomplicated TKA? Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA;. 19(9), 1411-7.
- 2.Bourne R B, Chesworth B M, Davis A M, Mahomed N N, Charron K D. (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res;. 468(1), 57-63.
- 3.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on. between1981and1995 in Sweden. Acta Orthop Scand; 71(3), 262-7.
- 4.Kim T K, Chang C B, Kang Y G, Kim S J, Seong S C. (2009) Causes and predictors of patient’s dissatisfaction after uncomplicated total knee arthroplasty. , The Journal of arthroplasty; 24(2), 263-71.
- 5.Park K K, Shin K S, Chang C B, Kim S J, Kim T K.Functional disabilities and issues of concern in female Asian patients before TKA. Clinical Orthopaedics and Related Research. 2007(461), 143-52.
- 6.Lavernia C J, Alcerro J C, Rossi M D. (2010) Fear in arthroplasty surgery: the role of race. , Clin Orthop Relat Res; 468(2), 547-54.
- 7.Ranawat C S, Ranawat A S, Mehta A. (2003) Total knee arthroplasty rehabilitation protocol: what makes the difference? The Journal of arthroplasty;18(3Suppl1):. 27-30.
- 8.Singelyn F J, Deyaert M, Joris D, Pendeville E, Gouverneur J M. (1998) Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesthesia and analgesia;. 87(1), 88-92.
- 9.Maheshwari A V, Blum Y C, Shekhar L, Ranawat A S, Ranawat C S. (2009) Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res;. 467(6), 1418-23.
- 10.Wheeler M, Oderda G M, Ashburn M A, Lipman A G. (2002) Adverse events associated with postoperative opioid analgesia: a systematic review. The journal of pain :. , official journal of the American Pain Society; 3(3), 159-80.
- 11.Shoji H, Solomonow M, Yoshino S, D’Ambrosia R, Dabezies E. (1990) Factors affecting postoperative flexion in total knee arthroplasty. , Orthopedics; 13(6), 643-9.
- 12.Perkins F M, Kehlet H. (2000) Chronic pain as an outcome of surgery - A review of predictive factors. , Anesthesiology; 93(4), 1123-33.
- 13.Chang C B, Cho W S. (2012) Pain management protocols, peri-operative pain and patient satisfaction after total knee replacement: a multicentre study. The Journal of bone and joint surgery Britishvolume;94(11):. 1511-6.
- 15.Kehlet H, Holte K. (2001) Effect of postoperative analgesia on surgical outcome. , British journal of anaesthesia; 87(1), 62-72.
- 16.Gibbs D M, Green T P, Esler C N. (2012) The local infiltration of analgesia following total knee replacement: a review of current literature. The Journal of bone and joint surgery Britishvolume;94(9):. 1154-9.
- 17.Davies A F, Segar E P, Murdoch J, Wright D E, Wilson I H. (2004) Epidural infusion or combined femoral and sciatic nerve blocks as perioperative analgesia for knee arthroplasty. British journal of anaesthesia;. 93(3), 368-74.
- 18.Parvizi J, Miller A G, Gandhi K. (2011) Multimodal pain management after total joint arthroplasty. The Journal of bone and joint surgery American volume;. 93(11), 1075-84.
- 19.Niemelainen M, Kalliovalkama J, Aho A J, Moilanen T, Eskelinen A. (2014) Single periarticular local infiltration analgesia reduces opiate consumption until 48 hours after total knee arthroplasty. A randomized placebo-controlled trial involving 56 patients. , Acta orthopaedica; 85(6), 614-9.
- 20.Ranawat A S, Ranawat C S. (2007) Pain management and accelerated rehabilitation for total hip and total knee arthroplasty.TheJournalofarthroplasty;22(7Suppl3):. 12-5.
- 21.Noyes F R, Fleckenstein C M, Barber-Westin S D. (2012) The development of postoperative knee chondrolysis after intra-articular pain pump infusion of an anesthetic medication: a series of twenty-one cases. The Journal of bone and joint surgery Americanvolume;. 94(16), 1448-57.
- 22.Kerr D R, Kohan L. (2008) Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. , Acta orthopaedica; 79(2), 174-83.
- 23.Kelley T C, Adams M J, Mulliken B D, Dalury D F. (2013) Efficacy of multimodal perioperative analgesia protocol with periarticular medication injection in total knee arthroplasty: a randomised, double-blinded study. , The Journal of arthroplasty; 28(8), 1274-7.
- 24.Vendittoli P A, Makinen P, Drolet P, Lavigne M, Fallaha M et al. (2006) A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. The Journal of bone and joint surgery Americanvolume;. 88(2), 282-9.
- 25.Fu P L, Xiao J, Zhu Y L, Wu H S, Li X H et al. (2010) Efficacy of a multimodal analgesia protocol in total knee arthroplasty: a randomized, controlled trial. , The Journal of international medical research; 38(4), 1404-12.
- 26.MAKM Ritter, Keating E M, Faris P M, Meding J B. (1999) Intra-articular morphine and/or bupivacaine after total knee replacement. , J Bone Joint Surg Br; 81, 301-3.
- 27.Kehlet H, Andersen L O. (2011) Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. , Acta anaesthesiologica Scandinavica; 55(7), 778-84.
- 28.Andersen L O, Kristensen B B, Husted H, Otte K S, Kehlet H. (2008) Local anesthetics after total knee arthroplasty: intraarticular or extraarticular administration? A randomized, double-blind, placebo-controlled study. , Acta orthopaedica; 79(6), 800-5.
- 29.Oshima Y. (1995) Postcolumn Derivatization Liquid-Chromatographic Method for Paralytic Shellfish Toxins. , J Aoac Int; 78(2), 528-32.
- 30.Lagos N. (1998) Microalgal blooms: A global issue with negative impact in Chile. , Biol Res; 31(4), 375-86.
- 31.Lagos N. (2003) Paralytic shellfish poisoning phycotoxins: Occurrence in South America. , Comments on Toxicology; 9(2), 175-93.
- 32.Catterall W A. (1993) Structure and function of voltage-gated ion channels. Trends in neurosciences;. 16(12), 500-6.
- 33.Goldin A L. (2001) Resurgence of sodium channel research. Annual review of physiology;. 63, 871-94.
- 34.Strichartz G R, Hall S, Magnani B, Hong C Y, Kishi Y et al. (1995) The potencies of synthetic analogues of saxitoxin and the absolute stereoselectivity of decarbamoyl saxitoxin. Toxicon :. , official journal of the International Society on Toxinology; 33(6), 723-37.
- 35.Catterall W A. (2000) From ionic currents to molecular mechanisms: the structure and function of voltage-gated sodium channels. , Neuron; 26(1), 13-25.
- 36.Andrinolo D, Michea L F, Lagos N. (1999) Toxic effects, pharmacokinetics and clearance of saxitoxin, a component of paralytic shellfish poison (PSP), in cats. Toxicon :. , official journal of the International Society on Toxinology; 37(3), 447-64.
- 37.Lagos M. (2000) ADParalytic shellfish poisoning (PSP): Toxicology and Kinetics.In: Botana LM,editor.Seafood and freshwater toxins: Pharmacology, physiology and detection. First Edition. ed. New York-Basel.:MarcelDekker; 203-15.
- 38.Andrinolo D, Iglesias V, Garcia C, Lagos N. (2002) Toxicokinetics and toxicodynamics of gonyautoxins after an oral toxin dose in cats. Toxicon :. , official journal of the International Society on Toxinology; 40(6), 699-709.
- 39.Lagos N.(2014) Clinical Applications of Paralytic Shellfish Poisoning Toxins. In:. Toxins and Biologically Active Compound from Microalgae.In: Rossini GP, editor.Toxins and Biologically Active Compounds from Microalgae, Volume 2: Biological Effects and Risk Management:CRCPress; 309-29.
- 40.WHO. (2011) WHO Standards and operational guidance for ethics review of health-related research with human participants. , Geneva, Switzerland:, WHO Document Production Services; 56.
- 41.Hinzpeter J, Barrientos C, Zamorano A, Martinez A, Palet M et al. (2016) Gonyautoxins: First evidence in pain management in total knee arthroplasty. Toxicon :. , official journal of the International Society on Toxinology; 119, 180-5.
- 42.Ekberg J, Adams D J. (2006) Neuronal voltage-gated sodium channel subtypes: key roles in inflammatory and neuropathic pain. The international journal of biochemistry & cell biology;. 38(12), 2005-10.
- 43.Strickland I T, Martindale J C, Woodhams P L, Reeve A J, Chessell I P et al. (2008) Changes in the expression of NaV1.7, NaV1.8 and NaV1.9 in a distinct population of dorsal root ganglia innervating the rat knee joint in a model of chronic inflammatory joint pain. European journal of pain;. 12(5), 564-72.
Cited by (1)
- 1.Hinzpeter Jaime, Barahona Maximiliano, Aliste Julián, Barrientos Cristian, Zamorano Alvaro, et al, 2023, Gonyautoxins 2/3 Local Periarticular Injection for Pain Management after Total Knee Arthroplasty: A Double-Blind, Randomized Study, The Journal of Knee Surgery, 36(04), 389, 10.1055/s-0041-1735312
