Abstract
Untreated dental caries in children is one of the most common diseases and largest public health problems in the world. A novel caries management program, using 50% silver nitrate, 38% silver diamine fluoride, and 5% sodium fluoride varnish, was developed at Shoreview Dental, LLC, a private dental practice in Oregon USA, and then introduced into schools in Ecuador, Ghana, and Bolivia. Cavitated carious lesions were treated with 50% silver nitrate, followed by covering with 5% sodium fluoride varnish, three times over two weeks for 165 children in Ecuador at initial assessment, 3 months, and 6 months. This protocol was repeated for 271 children in Ghana at initial assessment and 12 months. In Bolivia, 130 children were treated with 38% silver diamine fluoride, followed by covering with 5% sodium fluoride varnish, once per visit at initial assessment, 6, 12, 18, 24, 30, and 36 months. The percentage of children with active cavitated carious lesions at initial evaluation was 92.7% (Ecuador), 55.4% (Ghana), and 92.3% (Bolivia). The final arrest rate of treated surfaces was 98.8% (Ecuador), 67.6% (Ghana), and 90.2% (Bolivia). Effectiveness of cavitated caries lesion arrest is increased when it is thoroughly cleaned and dried before the treatment protocol. Further optimization is obtained when this protocol is repeated multiple times.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC, Republic of Macedonia.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Steven R. Duffin, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
Dr. Steven R. Duffin and Marcus L. Duffin are principle members of NoDK, LLC. This company focuses on the dissemination of the medical management of caries protocol to populations throughout the world. They are also authors and editors of the “SMART Oral Health: The Medical Management of Caries” textbook.
Citation:
Introduction
The term “caries” is used to represent a bacteria-mediated disease and the term “caries lesion” represents the physical manifestation of this disease at the tooth surface level. Untreated caries represents a major public health challenge that impacts more than half a billion children globally. 1, 2, 3 Differences in prevalence and severity of caries lesions exist in various regions throughout the world. There is an increasing prevalence of early childhood caries (ECC) in developing countries associated with sugar consumption from snacks and sugar sweetened beverages (SSB), which is often cheaper than water in some countries. These products are associated with globalization and the nutrition transition away from healthy lifestyles and diets. 1, 2, 5
In developing countries, a vast majority of caries lesions go untreated due to a limited dental workforce and limited access to expensive traditional dental restorative treatment. This situation applies especially in low-income and rural communities. 1, 2 There is a need for a low-cost, painless, quick, and effective caries lesion treatment utilizing minimal equipment that can be carried out by community outreach healthcare workers. 4
The medical management of caries utilizing silver nitrate (SN) was introduced between 1880 and 1908.6 For unknown reasons, this approach to treating tooth infections (caries lesions) with medicine was abandoned during the mid-twentieth century. The successful implementation of the medical management of caries protocol at the private dental practice Shoreview Dental, LLC in Keizer, Oregon, involving the placement of 25% SN (Gordon Labs) followed by 5% sodium fluoride varnish (FV) (Centrix, Fluorodose), was described in the Journal of the California Dental Association (CDA) in 2012.7 Shortly after that paper was published, Shoreview switched to the use of 50% SN, instead of 25% SN. The manufacturer of SN, Gordon Labs, offered a 50% version, and it was hypothesized that increasing the concentration of silver ions would result in quicker and more successful cavitated caries lesion arrest.4 Ultimately, more rapid and successful cavitated caries lesion arrest was observed in Shoreview Dental after this transition.
In the 1960’s, Dr. R. Yamaga and colleagues combined the benefits of silver and fluoride into one compound, 38% silver diamine fluoride (38% SDF) (Saforide).8 In 2014, 38% SDF was cleared to market by the FDA for sale and use in the US (Elevate Oral Care, Advantage Arrest).9 This product then appeared in the US market in 2015. Once cleared, the Shoreview Dental Clinic transitioned from the use of 50% SN to the use of 38% SDF. It has been shown that there is no significant difference between the caries lesion arrest rates for 25% SN followed by FV and 38% SDF.10
A majority of the current literature on the use of silver ion compounds for the arrest of caries lesions is based on the use of 38% SDF.11, 16 The literature that discusses effective caries lesion arrest properties of SN is historical.6, 10, 12
This is a case report on humanitarian efforts to introduce SN and SDF, followed by fluoride varnish, treatment protocols for children living in rural communities in Ecuador, Ghana, and Bolivia. These projects were accomplished in a professional manner through collaboration with schools and in partnership with parents, local community leadership, school officials and health authorities at both the national and local level. The purpose of these projects was to demonstrate the effectiveness of protocols based on the medical management of caries6, 7 such that local professionals would want to adopt these protocols in a culturally competent and sustainable fashion while meeting appropriate legal requirements. Manuals containing standard protocols for conducting international humanitarian dental projects have been outlined by the FDI and WHO.13, 14 Even though our team was unaware of these manuals before conducting our projects, our operational plan followed those guidelines very closely.
Materials and Methods
Procedures
All patients received comprehensive instructions on promoting healthy food choices and good oral hygiene practices. Toothbrushes were donated to all of the participating schools to help maintain good oral health. Examples of clinical treatment settings in Ecuador, Ghana and Bolivia can be seen in Figure 1. No removal of caries lesion tissue was conducted before application of 50% SN or 38% SDF followed by FV in any of the humanitarian projects. Removal of decayed tooth structure before treatment using silver ion compounds does not increase the caries lesion arrest rate.11,16 All children were instructed to not eat or drink for at least one hour after treatment and to not brush their teeth until the next day.
Figure 1.Examples of children being treated in Ecuador (a), Ghana (b), and Bolivia (c).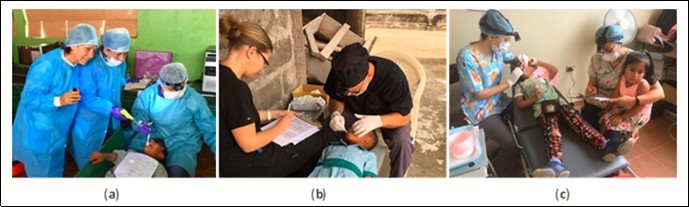
Ecuador
Following publication of the CDA paper in 2012, on the medical management of caries,7 two lead dentists from the Ecuador Ministry of Health contacted the dental team at Shoreview Dental, LLC. They then requested permission to come to the clinic and observe patient care using 50% SN followed by FV. Ecuador is a country with very high rates of caries lesion prevalence and severity in children.1,2 Following this visit in 2014, joint plans were made to conduct a humanitarian community outreach program for 165 students at the rural “Galapagos School”, located in the mountains near Ibarra. When the project began in 2015, the Shoreview Dental team’s role was to train dentists from our partner organization, the Ministry of Health, in application protocols and evaluation of cavitated caries lesion arrest outcomes. The Shoreview Dental team also provided the 50% SN and FV materials. Mobile dental equipment with a reliable compressed air source was provided by the Ministry of Health since access to electricity was available. After receiving training, Ministry of Health dentists conducted the charting, treatment, and outcome assessments. Ministry of Health Dentists were calibrated on-site by the Shoreview Dental team with hands-on training for the identification of arrested cavitated caries lesions based on the characteristics of a hard surface texture, as determined by gentle tactile examination, and black appearance.12,15 Consent forms were collected from the parents before treatment began. Due to the humanitarian nature of this project, IRB approval was not necessary.
The treatment protocol involved carefully cleaning with a toothbrush and thoroughly drying all cavitated caries lesions using compressed air, followed by the application of 50% SN (Gordon Laboratories) by scrubbing with a microbrush then covering with FV (Centrix, Fluorodose) to protect from saliva contamination. The lesions received three separate treatments over two weeks. This protocol of three treatments was repeated at three and six months. Intraoral images were collected for the maxillary and mandibular arches for all children at each time point (Figure 2 and Figure 3). Emergency services were both conducted on-site and via referral to local professionals. Simple extractions of abscessed teeth with local anesthesia were done on site. Referrals to the local Ministry of Health Dental Clinics were done in cases where endodontics and complex restorative procedures were necessary.
Figure 2.Example pre-treatment intraoral images for Ecuador (a), Ghana (b), and Bolivia (c) at initial evaluation.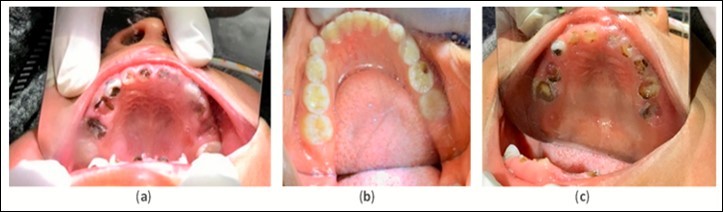
Figure 3.Example intraoral image of arrested cavitated caries lesions ost treatment.
Ghana
In early 2015, the Shoreview team was invited by the Paramount Chief, Nene Nuer Keteku III, and the Queen Mother, Manye Sebezo IV, of the Agotime Traditional Area located in the Volta region in Ghana, to conduct the same humanitarian program that was conducted in Ecuador. This was of particular interest since Ghana has such a low number of practicing dentists relative to the overall population.1,2 300 children from the “Comfort Gbetroh Memorial” school, located in the village of Kpetoe within the Volta region, participated in this project, with approval from the proprietress and head mistress Veronica Sadah. In September 2015, the Shoreview team arrived in Ghana and presented the project to the Ministry of Health, after which approval was received. Shortly afterwards, another presentation was conducted at the University of Ghana School of Dentistry, to faculty and students, to introduce the project and treatment methodologies used. After the presentations, the Shoreview team proceeded to the school to carry out the project. They conducted all of the charting, treatment, and cavitated caries lesion arrest outcome analysis throughout the project. They also provided the 50% SN (Gordon Laboratories), FV (Centrix, Fluorodose), and manually powered compressed air source, since there was no access to electricity in the school. Their ability to thoroughly air dry the lesion using the manually compressed air source, prior to treatment, was limited relative to what was used in Ecuador and Bolivia. Validation of cavitated caries lesion arrest was based on a hard surface texture, as determined by gentle tactile examination, and black appearance.12,15 Due to the humanitarian nature of this project, no IRB approval was necessary. Consent for treatment was received from the Paramount Chief and Queen mother, who are legally responsible for all children in the Agotime region.
The same materials, treatment frequency, and protocol used in Ecuador was replicated in Ghana. Evaluation and treatment were conducted at initial examination and at 12 months. Intraoral images of maxillary and mandibular arches were collected for all patients at each time point (Figure 2 and Figure 3) . At the 12-month visit, the Ghanaian dentist Dr. Ama Ofosu Appiah, our partnering individual, joined the Shoreview team and participated in the project. Her role was to assist in treatment and outcomes documentation. The Shoreview team calibrated this dentist in-person via hands-on training for the application protocol and cavitated caries lesion arrest assessment.
Emergency services were provided on-site where abscessed teeth were removed with local anesthesia at the school. School officials were instructed to find a nearby dentist to provide endodontics and complex restorative procedures when necessary. A surprising finding in this population was that most children had excellent oral health with very few cavitated caries lesions in their dentitions (Figure 2 and Figure 3).
Bolivia
In 2016, the Seattle based Non-Governmental Organization (NGO), Smiles Forever Foundation, in collaboration with the Shoreline Community College Dental Hygiene School, started a humanitarian project in Villa Tunari within the Chapare Amazon region of rural Bolivia. The chosen location for this project was the Maria del Rosario school, where a total of 130 children participated. The prevalence and severity of caries in Bolivian children is among the highest in the world, and is not that dissimilar from what was observed in Ecuador.1,2 Participating dentists, from the Smiles Forever Foundation Clinic in Cochabamba Bolivia, calibrated the dental hygiene teachers and students, from Shoreline Community College, at their clinic via hands-on training for proper protocol application and cavitated caries lesion arrest outcome assessment before traveling to Villa Tunari. At that point in time, all of the treatments and charting were conducted by the combined Smiles Forever Foundation and Shoreline Community College team. All materials throughout the project were provided by the Smiles Forever Foundation. This project involved one treatment per timepoint using 38% SDF followed by FV due to operational time constraints. Both Ecuador and Ghana involved three treatments per timepoint using 50% SN followed by FV. Cavitated caries lesion arrest was identified when the lesion was hard, as determined by gentle tactile examination, and black.12,15 Consent was obtained from school officials, parents, and the local hospital Oral Public Health Manager before treatment began. Due to the humanitarian nature of this project, no IRB approval was needed.
Just before the 6-month timepoint in early 2017, the Shoreview Dental, LLC team was invited to participate in this project. The Shoreview Dental, LLC team’s role, as a partner organization to Smiles Forever, was to provide further training on the proper identification of arrested cavitated caries lesions following treatment. Upon arrival, The Shoreview Dental, LLC team presented the topic of the medical management of caries to the Medical, Dental, and Public Health community at Universidad Prevada Abierto Latino America (UPAL) Dental University in Cochabamba. Following this presentation, UPAL faculty members decided to participate in the project. Their role was to observe and participate, as a partnering institution with Smiles Forever, in the treatment of cavitated caries lesions and identification of lesion arrest.
The treatment protocol used in Bolivia differed from what was used in Ecuador and Ghana. The protocol that was used involved the following: carefully clean the cavitated caries lesion using a toothbrush, thoroughly dry using compressed air, apply 38% SDF by scrubbing with a microbrush applicator, then cover with FV to prevent saliva contamination. Since access to electricity was available at the school, mobile dental equipment with a reliable compressed air source was available. This protocol was repeated at the timepoints of 6, 12, 18, 24, 30, and 36 months. Intraoral images of maxillary and mandibular arches were collected for all patients present at 36 months (Figure 2 and Figure 3). Emergency services were both conducted on-site and via referral to local professionals. If a tooth showed signs of being abscessed, it was extracted by Smiles Forever Clinic dentists on site using local anesthesia. Endodontics and complex restorative procedures were referred out to the local hospital dental department or the Smiles Forever Clinic in Cochabamba.
Explanation for Use of SN or SDF in Projects
The first project in Ecuador utilized 50% SN followed by FV in early 2015 because that was the established protocol at the Shoreview Dental, LLC dental clinic and 38% SDF was not yet cleared to market by the FDA. The same protocol used in Ecuador was utilized in Ghana in late 2015 for reasons of consistency. However, 38% SDF was used in Bolivia in 2016 because the Smiles Forever Foundation had started using it before Shoreview Dental, LLC officially became a part of the program. In addition, SDF was becoming more widely used due to FDA clearance, and there is more published literature about SDF when compared to SN.4,24
Data Analysis
Although these three humanitarian community outreach programs were not conducted as research, and should be looked at as separate case reports, careful attention to data collection was made at initial examination and at all follow up encounters. The Shoreview Dental, LLC team exclusively conducted data analysis on outcomes data related to Ecuador and Ghana but collaborated with the Smiles Forever Foundation for data analysis related to Bolivia. Surface specific charting and maxillary and mandibular arch photos were taken at all timepoints in Ecuador and Ghana but only at 36 months in Bolivia. A determination of all cavitated caries lesion activity or arrest was recorded based on lesion color and surface hardness. A lesion was considered arrested if the color was black and the surface was determined to be hard using gentle tactile examination (Figure 3).12,15 The presence or absence of caries lesion related mouth pain was asked of the children themselves as well as their parents and teachers.
Results
The results discussed below are derived from Table 1. Please review the table for a more comprehensive evaluation of outcomes. Pre-treatment intraoral image examples of cavitated caries lesions in Ecuador, Ghana and Bolivia can be found in Figure 2. An example of arrested cavitated caries lesions can be found in Figure 3. All charted information for all patients was stored securely and confidentially and data was anonymized before evaluation of outcomes.
Table 1. Longitudinal assessment of treatment effectiveness and the amount of new cavlated caries lesion formation in thr different humanitarian projec s, one site per country. Ecuador and Ghana received three treatments using 50% SN followed by while Bolivia only received one treatment using 38% SDF followed by FVduring each time point.| Ecuador | Ghana | Bolivia | ||||||||||
| Initial | 3 M | 6 M | Initial | 12 M | Initial | 6 M | 12 M | 18 M | 24 rs4 130 M | 36 M | ||
| Children | 165 | 158 | 161 | 271 | 206 | 130 | 104 | 60 | 37 | 33 32 | 22 | |
| %Children Absent | 0% | 4.20% | 2.40% | 0% | 24.00% | 0% | 20.00% | 53.80% | 71.50% | 74.6% 75.4% | 83.10% | |
| 96 Children with Active Cavitated Caries Lesions | 93.90% | 8.90% | 25.50% | 43.20% | 26.20% | 95.40% | 85.60% | 73.30% | 56.8% | 90.996 1 | 65.60% | 68.20% |
| Non-arrested Teeth | 930 | 8 | 9 | 385 | 82 | 947 | 221 | 87 | 28 | 27 | 26 | 15 |
| Non-arrested Surfaces | 1,626 | 11 | 14 | 455 | 99 | 1117 | 247 | 94 | 29 | 28 | 27 | 15 |
| New Decayed Teeth | 0 | 11 | 69 | 0 | 75 | 0 | 194 | 159 | 30 | 81 | 31 | 41 |
| New Decayed Surfaces | 0 | 15 | 88 | 0 | 147 | 0 | 270 | 197 | 34 | 104 | 40 | 70 |
| Average Decayed Teeth | 5.6 | 0.1 | 0.5 | 1.4 | 0.8 | 7.3 | 4 | 4.1 | 1.6 | 3.3 | 1.8 | 2.5 |
| Average Decayed Surfaces | 9.9 | 0.2 | 0.6 | 1.7 | 1.2 | 8.6 | 5 | 4.9 | 1.7 | 4.0 | 2.1 | 3.9 |
| Arrested Teeth | 0 | 864 | 839 | 0 | 210 | 0 | 594 | 471 | 383 | 342 | 339 | 185 |
| Arrested Surfaces | 0 | 1399 | 1333 | 0 | 243 | 0 | 688 | 519 | 404 | 380 | 411 | 211 |
| % Arrested Teeth | 0% | 99.1% | 98.90% | 0% | 71.90% | 0% | 72.90% | 84.4% | 93.2% | 92.7% | 92.90% | 92.50% |
| %Arrested Surfaces | 0% | 99.2% | 99.00% | 0% | 71.10% | 0% | 73.60% | 84.7% | 93.3% | 93.1% | 93.80% | 93.40% |
Ecuador
A total of 165 children, ranging from 3 to 18 years old, attended initial evaluation where 93.9% of the children had active cavitated caries lesions. The average number of teeth with active cavitated lesions was 5.6 at the initial evaluation and 0.5 at the final evaluation (6 months). The average number of surfaces with active cavitated lesions was 9.9 at the initial evaluation and 0.6 at the final evaluation. The arrest rate for teeth with cavitated caries lesions was 98.9% at the final evaluation. The arrest rate for tooth surfaces with cavitated caries lesions was 99.0% at the final evaluation.
Ghana
A total of 271 children, ranging from 3 to 14 years old, attended initial evaluation where 43.2% of the children had active cavitated caries lesions. The average number of teeth with active cavitated lesions was 1.4 at the initial evaluation and 0.8 at the final evaluation (12 months). The average number of tooth surfaces with active cavitated lesions was 1.7 at the initial evaluation and 1.2 at the final evaluation. The arrest rate for teeth with cavitated caries lesions at the final evaluation was 71.9%. The arrest rate for tooth surfaces with cavitated caries lesions at the final evaluation was 71.1%.
Bolivia
A total of 130 children, ranging from 4 to 16 years old, attended the initial evaluation where 95.4% of the children had active cavitated caries lesions. The average number of teeth with active lesions was 7.3 at the initial evaluation and 2.5 at final evaluation (36 months). The average number of surfaces with active cavitated caries lesions was 8.6 at the initial evaluation and 3.9 at the final evaluation. The arrest rate for teeth with cavitated caries lesions was 72.9% at the first follow-up (6 months) and 92.5% at the final evaluation. The arrest rate for tooth surfaces with cavitated caries lesions was 73.6% at the first follow-up and 93.4% at the final evaluation.
Comparison Summary
Both Ecuador and Ghana programs utilized the same treatment protocol involving three treatments per visit using 50% SN followed by FV for a total of nine treatments over six months in Ecuador and six treatments over 12 months in Ghana. However, there was a difference between the percentage of arrested cavitated caries lesions. Ecuador had a final tooth surface arrest rate of 99.0% while Ghana had a final tooth surface arrest rate of 71.1%. Ecuador also received three treatments at 3-month intervals over 6 months while Ghana received three treatments at initial and 12 months. The Bolivian program utilized a treatment protocol that involved one treatment per visit of 38% SDF followed by FV at 6-month intervals, for a total of seven treatments over 36 months, and had a final tooth surface arrest rate of 93.4%.
Discussion
The percent of children with active cavitated caries lesions in Ecuador, Ghana and Bolivia at the initial evaluation was 93.9%, 43.2%, and 95.4% (Table 1). This is likely due to the nutrition transition based on the earlier arrival of junk food and sugar sweetened beverages (SSB) in Latin America (1980s and 1990s) and later in Ghana (2000s).17 These differences could also be due to different oral hygiene practices, genetic differences between populations, levels of naturally occurring fluoride in the local water supply, low cost of high sugar products and/or oral microbiome composition.
One commonality that was observed across all three countries was the sale of junk food, candy, and SSB in and/or around the schools (Figure 4). Often, the children were snacking throughout the day at school and many of them had untreated tooth decay. This high level of tooth decay was likely due to a limited dental care workforce, low access to care in rural areas, high cost of traditional restorative care and low prioritization of preventive dental care.4 This is especially true for children because, as stated by the pediatrician Dr. Karen Sokal-Gutierrez, it is commonly believed that “baby teeth do not matter since they fall out anyway” (K Sokal-Gutierrez, MD, MPH, oral communication, 2017). It was also possible that they did not have access to fluoridated water, but that was not a metric that was measured. These observations suggest that there is a fundamental need to focus on promoting healthy nutrition for children to help prevent non-communicable diseases such as dental caries, obesity, type 2 diabetes, and cardiovascular disease.18
Figure 4.Examples of Candy Stores in Bolivia (a) and Ghana (b) Schools.
When analyzing the effectiveness of the treatment protocols used in these countries, it was hypothesized that the high level of success in cavitated caries lesion arrest rates, as seen in Ecuador and Bolivia, may be due to the application protocol. The similar rates of cavitated caries lesion arrest between Ecuador and Bolivia show that the 50% SN followed by FV protocol provides similar results to the 38% SDF followed by FV protocol.10 The strategy used was based on experience obtained over many years in the Shoreview Dental Clinic.7 The best outcomes were observed when multiple treatments were done using silver ion compounds4 followed by FV on active cavitated caries lesions that were thoroughly cleaned using a toothbrush and dried using compressed air before treatment. Even better outcomes were observed when those multiple treatments were performed over a short period of time, as exhibited in Table 1, when comparing Ecuador and Bolivia outcomes data. Since Ecuador had a lower amount of active cavitated caries lesions than Bolivia at the final evaluation, it suggests that multiple treatments over a short period of time decreases the rate of new cavitated caries lesion formation. These observations demonstrate that a dose response curve phenomenon could be occurring based on differences in application protocols for these three humanitarian projects.
It is hypothesized that Ecuador had a higher rate of cavitated caries lesion arrest than Bolivia due to the following points: The Ecuadorian Ministry of Health dentists received hands on training at the Shoreview Dental, LLC clinic and Shoreview staff provided further training on-site in Ecuador. The same dentists also participated at each treatment date. In Bolivia, treatment and charting was done by Bolivian dentists and dental hygienists as well as dental hygiene students and instructors from the US. The students rotated between treatment stations and their composition varied from year to year. This could have resulted in some variation of protocol and charting consistency due to the complex nature of managing all of the various providers.
In Ghana, there was no electricity available for compressed air and the manually powered compressed air system used had some limitations in obtaining total lesion desiccation prior to the application of 50% SN followed by FV. In Shoreview Dental’s experience, removing saliva contamination from the lesion using compressed air, before the application protocol, is critical to obtaining a high level of success. It is hypothesized that saliva contamination prevents the silver ion from penetrating deep into the lesion via capillary action. The proteins in saliva may also sequester away the silver ions due to the reactive/chemical nature of ionic silver. It is possible that the limited ability to thoroughly dry the cavitated caries lesions in Ghana resulted in a lower arrest rate when compared to Ecuador and Bolivia, where consistent access to compressed air was available.
To further prevent saliva contamination, patients were instructed to not eat or drink for at least one hour after treatment and to not brush their teeth until the next day. It is hypothesized that the application of FV over 50% SN or 38% SDF provides a hydrophobic barrier for saliva. Eating or drinking right after treatment could physically remove that barrier and allow for saliva contamination, depending on the diet. Not brushing their teeth until the next day adds another level of protection from the physical removal of FV. The longer the FV is undisturbed, the greater the likelihood that the treated cavitated caries lesion would remain uncontaminated by saliva, giving the silver ions more time to interact with and penetrate deeper into the lesion.
On follow up visits in Ecuador, Ghana, and Bolivia, parents and teachers reported that the children who were treated in this manner experienced less mouth pain. They also stated that there was little concern about the black stain on the treated lesion. This corresponds with earlier observations at the Shoreview Dental, LLC clinic.
In Bolivia, some patients had their arrested cavitated caries lesions, which were black and hard to the touch, covered with glass ionomer cement in the anterior aesthetic zone or on large lesions in posterior teeth. This kind of intervention has come to be known as Silver Modified Atraumatic Restorative Treatment (SMART).19, 20 This was done only in cases where the patient and parent had aesthetic concerns or the lesion would result in a food trap.
Recent additions to the literature suggest that a shift is taking place in the dental profession towards prevention and minimal intervention.4, 21, 22, 23 Prior to this shift, surgical restorative techniques were often used as the first response to the presence of a caries lesion. When using the medical management of caries protocol, it is not necessary to remove any decayed tooth structure. It has been shown that the removal of decayed tooth structure does not provide any added benefit to the arrest rate of active caries lesions when following this protocol.11, 16
Conclusions
The dramatic difference in severity of tooth decay between school children living in Ghana (low) and Ecuador/Bolivia (high) is worthy of further investigation.
Preventing saliva contamination by thoroughly drying the cavitated caries lesion before treatment appears to be critical in obtaining a high level of success in cavitated caries lesion arrest, as observed in the humanitarian project in Ghana. The FV may provide a hydrophobic barrier to saliva contamination for the treated surface. It is hypothesized that the longer the varnish remains on the lesion after treatment, the lower the chance of saliva contamination and the higher the chance of active cavitated caries lesion arrest. Ensuring that the patients do not eat or drink for at least one hour after treatment and wait until the next day before they brush their teeth may help in further preventing saliva contamination.
Providing three treatments in a short period of time (Ecuador: nine total treatments at 3-month intervals over 6 months) versus only one treatment (Bolivia: 7 total treatments at 6 month intervals over 36 months) improves the cavitated caries lesion arrest outcomes. A similar level of cavitated caries lesion arrest was observed when comparing treatment protocols using 50% SN followed by FV and 38% SDF followed by FV. The literature had previously shown that the application of 25% SN followed by FV provides similar results to the application of 38% SDF.10 Further confirmation of success using these treatment protocols await future clinical trials.
The effective and low-cost cavitated caries lesion intervention, using silver ion compounds followed by FV, should be given high consideration in future oral health programs. The caries lesion arrest properties of these interventions have been well documented.22, 24, 25 Prevention properties of this non-invasive approach to care have been identified as a side effect in many caries arrest studies.4, 26 However, there remains opportunities to examine this phenomenon separately.
Author Contributions
Both Dr. Steven R. Duffin and Marcus L. Duffin contributed to conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing—original draft preparation, writing-review and editing, visualization, supervision, project administration, and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
These projects received no external funding.
Acknowledgments
We would like to thank the following people for their important contribution to the operational logistics of these three projects: Dr. Ama Ofosu Appiah DDS, Dr. Seneida Benitez, Fraser Bullock MBA, Jacqueline Juhl BS RDH MS, Tiffani Ann Kealiher EFDA, Sandy Kemper RDH, Philippe Kradolfer, Dr. Galud Pinto, Jonalee Potter BSDH RDH EPP MHA, Dr. Nayda Apata Rojas and Veronica Sadah. We would also like to thank Dr. Karen Sokal-Gutierrez MD MPH for her editorial assistance and Mauricio Ramirez for his data analysis contributions.
References
- 1.Robeaglehole R, Benzian H, Crail J, Mackay J. (2009) The oral health atlas mapping a neglected global health issue. FDI World Dental Federation.
- 2. (2016) The future of oral health: global challenges, advances, and new technologies. Scientific American Custom. , Media
- 3.Kassebaum N J, AGC Smith, Bernabe E, Fleming T D. (2017) Global, regional, and national prevalence, incidence and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. , JDR 96, 380-387.
- 4.Sultan A. (2019) Silver diamine fluoride as a proactive anti-caries tool: a review. , Int J Oral Hlth Dent 5(2), 63-68.
- 5.Anil S, Anand P. (2017) Early childhood caries: prevalence, risk factors, and prevention. Front in Ped. 5(18)
- 6.Black G V. (1908) A work on operative dentistry the pathology of the hard tissues of the teeth. , Chicago: Medico-Dental Publishing Company 1(1), 235-257.
- 7.Duffin S. (2012) Back to the future: the medical management of caries introduction. , J Calif Dent Assoc 40(11), 852-858.
- 8.Yamaga R, Nishino M, Yoshida S, Yokomizo I. (1972) Diammine silver fluoride and its clinical application. , J Osaka Univ Dent S 12, 1-20.
- 10.Gao S, Zhao I, Duffin S, Duangthip D, Lo E et al. (2018) Revitalising silver nitrate for caries management. , Int J Envir Res Pub Hlth 15(1), 80.
- 11.Chu C H. (2002) Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in chinese pre-school children. JDR. 81(11), 767-770.
- 12.Howe P R. (1917) A method of sterilizing and at the same time impregnating with a metal, affected dentinal tissue. , Philadelphia: S S White Dental Manufacturing Company 59, 891-904.
- 13.WVP Helderman, Lo E, Holmgren C. (2003) Guidance for the planning, implementation and evaluation of oral health care demonstration projects for under-served populations. Int DentJ.19-25.
- 14.Frencken J E, Holmgren C, Helderman V P. (2002) WHO Basic Package of Oral Care (BPOC).Nijmegen, Netherlands: WHO Collaborating Centre for Oral Health Care Planning and Future Scenarios,University of Nijmegen.
- 15.Horst J. (2016) UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 44(1), 16-28.
- 16.Crystal Y, Niederman R. (2019) Evidence-based dentistry update on silver diamine fluoride. Dent Clin North Am. 63(1), 45-68.
- 17.Popkin B M. (2001) Nutrition in transition: the changing global nutrition challenge. , Asia Pac J Clin Nutr 10, 13-18.
- 18. (2002) Diet, nutrition and the prevention of chronic diseases. Report of a joint WHO/FAO expert consultation. WHO. WHO Technical Report Series 916 , Geneva, Switzerland.:
- 19.Duffin S, Duffin M, Juhl J, Schwab J. (2019) SMART Oral Health: The Medical Management of Caries.Kindle DirectPublishing.
- 20.Seifo N. (2020) The use of silver diamine fluoride (SDF) in dental practice. , BDJ 228(2), 75-81.
- 21.NPT Innes. (2019) A century of change towards prevention and minimal intervention in cariology. JDR. 98(6), 611-617.
- 22. (2018) Caries management clinical practice guidelines (2018–2022). American Dental Association;. ebd.ada.org/en/evidence/guidelines/caries-management#
- 23.Cohen L, Dahlen G, Escobar A, Fejerskov O, Johnson N et al. (2017) The future of oral health dentistry in crisis – time for change.
- 24.Mei M L, ECM Lo, Chu C H. (2018) Arresting dentine caries with silver diamine fluoride: what’s behind it?. , JDR 97(7), 751-758.
