Abstract
Uganda still grapples with a high maternal mortality rates of 336 deaths per 100,000. Expectant mothers across the country lack awareness about the availability of antenatal care services; yet attendance of antenatal care services during pregnancy is crucial in protecting the health of women and unborn children. This article describes a protocol for investigating the effectiveness of mobile telephone communication interventions on the utilization of antenatal care services among expectant mothers in the districts of Kyotera and Rakai Districts in Uganda. Under the protocol, 28 health facilities in the districts of Kyotera and Rakai will be selected using simple random sampling and allocated into the intervention and control arms at a ratio of 1:1. A total of 2224 expectant mothers receiving antenatal care from the sampled health facilities will be recruited using systematic sampling. Expectant mothers receiving antenatal care from facilities allocated into the intervention arm will receive mobile telephone voice and text messages reminders for scheduled ANC visits. The mobile telephone messages will further provide maternal health information and availability of ANC services on a fortnightly basis.
On the other hand, expectant mothers receiving antenatal care from facilities allocated into the control group will not get any reminders for scheduled ANC visit and maternal health information through the mobile telephone communication platform. Expectant mothers in the control arm will receive standard maternal health care without reminders.
Expectant mothers in both groups will provide baseline data, midterm data will be obtained from the ANC registers at 6 moths while end of term data will be collected after an intervention period of 12months. The data collected will include the number of antenatal care visits attended, antenatal care services obtained from the health facilities, sociodemographic factors and mobile telephone usage, ownership and knowledge. The anticipated outcomes are; increased awareness and utilization of ANC services.
Author Contributions
Academic Editor: Ian James Martin, Edith Cowan University, USA
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Maria Nakachwa, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Effective doctor-patient communication is an integral part of clinical practice and an essential component in building of the doctor-patient relationships. Studies have shown that the approach adopted by health workers to communicate information is equally important as the actual information that is being communicated1.
Similarly, maternal health care requires effective communication between expectant mothers and the healthcare systems. The Sustainable Development Goals prioritize improvement of maternal health with a target of reducing the global maternal mortality to less than 70 per 100000 live births by the end of the year 20302. The prioritization of maternal health on the UN agenda is not accidental because globally, approximately 810 women die every day from preventable causes related to pregnancy and childbirth3. Majority of these deaths ((94%) occurred in low-resource settings yet most could have been prevented3.
In the some of the developed economies such as the United States of America, approximately 700 women across the United States of America (U.S.A) die each year as a result of pregnancy or pregnancy-related complications yet over 60% of pregnancy-related deaths are avoidable4. Lack of knowledge on warning signs and need to seek care are identified as major factors contributing to the death of expectant mothers. In Latin America, studies emphasize that countries need to strengthen their work at the community level to track pregnant women and encourage them to attend all four recommended ANC visits; this is in addition to consideration of interventions such as using new technologies like text messages to a woman’s cell phone or the phone of a family member5.
There was a noticeable decrease in the global MMR to 216/1000006. However, the African continent is still confronted with a high MMR of 542/100000 with the West African Region having a slightly higher MMR (515/100,000) compared to the other African Regions. Nigeria largely contributes to the West African Region value with an MMR of 814/100000 with the leading causes identified as underutilization of ANC services and inadequacy of facilities estimated at 47.5% and 92.6%, respectively7.
The East African Region has an average estimated MMR of 515/100000 with Southern Sudan having the highest MMR of 789/100000. Notably, the East African has a high MMR compared with other regions around the world6. This means that more maternal deaths happen in the East African region. A recent study in Rwanda indicates that majority of expectant mothers in (54%) women still do not complete the recommended number of four visits to ANC during pregnancy and recommends raising general awareness in communities on the importance of number and timing of ANC visits particularly among pregnant women and their husbands8.
Studies in Uganda indicate that attendance and utilization of antenatal cares service is still low with most women registering late ANC attendance averagely 5.5moths of pregnancy and non-completion of the required four visits9. The need to conduct sensitization about availability of ANC services specifically in rural areas to empower pregnant women and their husbands to improve ANC attendance and utilization is considered a viable option9. Sensitization can notably take on different forms including but on limited to print and digital media that will be explored in the current study with the use of mobile telephone services.
Reports from the Uganda Health Ministry indicated that maternal mortality continued to be a major challenge in regional referral hospitals10. The facility-based MMR for RRHs in FY 2016/17 was 350 per 100,000 hospital deliveries compared to 343 per 100,000 in 2015/16. Fort Portal, Hoima and Soroti RRHs had the highest MMR of 719, 693 and 618 per 100,000 respectively while Gulu and Kabale had the lowest MMR of 48 and 63 per 100,000 respectively.
Furthermore, findings showed that Bunyoro and Bugisu sub-regions had the lowest percentage of women who had had four or more ANC visits (45 percent and 47 percent, respectively)11. This could partly explain the high MMR in Hoima and Soroti Regional Referral Hospitals10.
The percentage of women in Uganda who had four or more ANC visits for their most recent birth in the 5 years preceding the 2016 demographics survey increased greatly with women’s education10. Among women with no education, 53 percent went on four or more ANC visits compared with 72 percent of women with more than a secondary education. The proportion of women with four or more ANC visits also increases with household wealth.
Uganda targeted to increase the utilization of ANC services to 47.5% by the end of the year 2020 and attain a maternal mortality ration of 211/100000 live births12. However, the ANC uptake stagnated and at 42%13. This could explain why the MMR stagnated at 336/100000 live births. Rural based studies in western Uganda provide an estimated MMR of 270/100000 live births14. This is notably high considering the desired national target. Recent studies in the rural Rakai District indicate that forty-four percent (44%) of expectant mothers deliver at home, 17% at traditional birth attendant’s (TBA) place, 32% at public health units, and 7% at private clinics15. The aggregation of home deliveries and TBA deliveries leads to 61% of deliveries that are not attended to by skilled health personnel. This notably depicts underutilization of maternal health services by expectant mothers in the districts Kyotera and Rakai that continues to expose mothers to maternal morbidity and mortality.
Poor communication and high transport costs are among the factors that contribute to the underutilization of ANC services among expectant mothers in Kyotera and Rakai Districts 14.
Closely related reports indicate that Rakai District was one of the districts whose health performance indicators had declined; for instance, only 1,659 expectant mothers out of the 5,589 estimated pregnancies in Rakai District received ANC services10. The low levels of ANC utilization are attributed to lack of awareness among expectant mothers that continues to expose expectants mother’s risks that arise from home and TBA deliveries
It is asserted that there is the need for more community-based interventions geared at mobilizing the community to adapt early health seeking behaviors such as ANC attendance during the first trimester13. This means that there are maternal information gaps among expectant mothers that must be addressed though effective community mobilization strategies such as use of available technologies.
There is a noticeable gap in the consumption of ANC services among expectant mothers in Rakai District with only 39% of expectant mothers receiving ANC services against the desired national consumption of 47.5% 15. The gap in in the utilization of ANC services arises from the inadequate maternal health information that is availed to expectant mothers in the districts of Kyotera and Rakai 13. This continues to exposes mothers to all risks associated with home and TBA deliveries that culminates into maternal morbidity and mortality.
Materials and Methods
Study Design
The study will deploy an experimental research design to assess the effect mobile telephone communication on the utilization of ANC services during pregnancy in the districts of Kyotera and Rakai Uganda. The Cluster Randomized Controlled Trial (CRCT) design comprised of both quantitative and qualitative approaches will be used as a gold standard in conducting this impact evaluation research in order to maximize comparability between the intervention and control groups, and hence give a strong evidence of a causal relationship between the intervention and the outcome 16, 17, 18.
The 28 health centres will formulate the units of randomization; a total of 2214 expectant mothers obtaining ANC services from the selected health centres will be recruited into the study by systematic sampling.
Therefore, the selected health centres (clusters) will be randomly assigned to either the intervention or control arm of the study leading 14 health centres in the intervention and 14 health centres in the control arm.
A single blinded approach will be implemented to prevent systematic biases arising from prior knowledge of group allocations among the participants and research aim outcomes as per RCT study standards17. Information regarding research hypotheses and randomization of health Centres into the different study arms research assistants, expectant mothers and cluster team leaders to avoid biases at the different levels of research.
The study will use the Intent to Treat (ITT) approach for analysis to minimize biases and establish the actual effect of mobile telephone communication. In the ITT, every expectant mother allocated to the intervention group is considered to be part of the trial. The study will make use of the pre-test-post-test control group approach18. In this approach, baseline characteristics regarding mobile telephone communication and utilization of ANC services will be collected from expectant mothers from both arms of the study to allow for a discrete evaluation of the pre-to-post changes.
Qualitative data will be collected through focus group discussions with expectant mothers, health workers, community leaders and VHT’s. Additional qualitative data will be obtained from in-depth interviews of key informants in the community such as district health officers, district chairpersons and leaders of VHT’s and midwives.
Study Variables
Independent Variable: Mobile Telephone Communication
Ownership
Knowlede and Usage
Voice/Text/Recorded Messages
Dependent Variable: Antenatal Care Services Utilization
Uptake of ANC
Examination ANC Services
Testing ANC Services
Treatment ANC Services
Non uptake of ANC
Mediating Variable: Expectant Mother Factors
Social Demographic Factors
Economic Factors
Accessibility Factors
Pregnancy Related factors
Study Setting
The study will be conducted in Kyotera and Rakai Districts found in the central region of Uganda20. Kyotera District lies approximately 44km, by road, south west of Masaka District. It is also 29km, by rod, northeast of Rakai District. The coordinates for Kyotera District are 0037'54.0” S,31032'36.0E. The district headquarters are located at Kasaali (Vote: 621). Similarly, Rakai district is located in South Western Uganda. It is west of Lake Victoria, lying between longitude 310E, 32oE and latitude0oS. The southern boundaries of Rakai are part of the international boundary between Uganda and Tanzania. It is bordered by Masaka District in the East, Kalangala District in the South-East, Isingiro District in the West and Lyantonde District in the North. The district headquarters are located in Rakai Town which is a tarmac road distance of approximately 190km from Kampala the Capital City of Uganda, it has a total area of 7908.7 sq/km with a total population of 518,008 people comprising of 253,054 males and 264,954 females20. Out of the 264,954 females, 158,972 females are above 15 years of age with an estimate fertility rate of 6.2%21. It is thus anticipated that some of the study participants will be teenage mothers. The districts have 2 government hospitals, 01 health center IV, 22 health center III’s, 43 health center II and 49 not for profit health centers spread across the 20 sub-counties in Rakai District20. It is important to note that the population statistics and health facilities recorded are as per the population census of 2014 when Kyotera District was an integral part of Rakai District.
Study Population
2214 expectant mothers aged 15 to 49 years residing in the districts of Kyotera and Rakai in Uganda.
Inclusion and Exclusion Criteria for Expectant Mothers
The study will focus on expectant mothers in the districts of Kyotera and Rakai in Uganda. An expectant mother will qualify for inclusion in the study if the pregnancy is less than 10 weeks, she or a member of the household where she comes from owns a mobile phone and has willingness to participate. The Village Health Teams (VHT’s) will identify the potential trial participants. Participants who meet the eligibility criteria will be required to sign a consent form after obtaining the details of the study from the VHT’s. These will be randomized into either the intervention or control arms of the study depending on facility they obtain ANC services from. Participants in both arms will be followed for one year to establish the level of ANC uptake in light of predisposing, enabling and need factors. An expectant mother who falls short of the described criteria will certainly be excluded from the study.
Sample Size Calculation and Determination
The sample size will be calculated based on the formula in equation 1used for computing the number of individuals per arm assuming cluster level analysis for parallel RCT designs with dichotomous outcomes22.
The specific formula is provided in Equation 1.
m=(Z1-α/2 + Z1-β)2[p1 (1-p1)+p2 (1-p2)]/∆2 ……Equation 1
Where;
m=Desired sample size per group;
P1=the probability of an event happening in the control group which is the standard ANC service in Kyotera and Rakai Districts. Reports provide an annual estimate of 5,589 pregnancies in Kyotera and Rakai Districts and an estimate 1,659 expectant mothers utilizing ANC services within Kyotera and Rakai Districts10. This translates into an approximate ANC utilization of 30% among expectant mothers in Kyotera and Rakai Districts. Thus P1=0.3
P2=The probability of an event in the treatment group.
The MoH targeted to increase the level of consumption of ANC to 47.5% with different interventions such as sensitization 11. Thus P2=0.475.
∆= Represents the clinically important difference in the treatment proportions, P1-P2=-0.175
α=is the type one error (rejecting the null hypothesis when it is actually true). The study will deploy a two-sided t-test that requires smaller sample sizes and set α to 0.05
β=type two error (the probability of rejecting the null hypothesis when it is false). This is given by the power of the study. Conventionally, the power is set at 0.80, for higher the power, the more sample is required.
z= the standard normal deviate for a one or two sided x;
First Step:
Feeding the stated quantities into equation 1 yields the following;
Formula for determining the number of subjects per group for dichotomous outcomes for a two-sided significance level α and power 1-β we have;
m=(1.96+0.842)2 (0.3(1-0.3)+0.47(1-0.47))/(0.3-0.47)2
…………………….Equation 1
m=287 participants per study arm (Sample size before adjusting for the design effect)
Second Step:
In order to adjust for the clustering effect, the sample size for binary outcomes will be inflated by the Design Effect (DE) to obtain an adjusted sample size17.
The adjusted cluster size will thus be:
m={(Z1-α/2 + Z1-β)2(p1 (1-p1)+p2 (1-p2)]}/∆2x (1+(n-1)p)
……………………… Equation 2
The design effect is computed as; DE=1+(n-1)ρ
Where n is the number of individuals per cluster andρ the Intra-Cluster Correlation Coefficient (ICC).
ICC is the ratio of the between-cluster variance to the total variance of an outcome variance and quantifies the correlation between the outcomes of any two individuals within the same cluster17.
Since there are no previously published study findings in Uganda documenting the ICC, an ICC of 0.01 will be adopted since it is within the recommended inter-quartile range ICC (0.011- 0.094) for previously undocumented ICC. Researchers recommend a minimum cluster size of 50 subjects per cluster to cater for secondary outcomes, therefore, a fixed cluster size of 80 expectant mothers will be considered for this study17.
Therefore, the design effect will be;
DE=1+ (287-1) *0.01
DE=3.86
When the quantities are fed into equation 2, the adjusted sample size that the study will engage is;
m={(Z1-α/2 + Z1-β)2[p1 (1-p1)+p2 (1-p2)]}/∆2x DE
……….……....Equation 2
m=(1.96+0.842)2(0.3(1-0.3)+0.47(1-0.47))/[0.3-0.47)2x 3.86
……….……....Equation 3
m=287×3.86=1107 (Sample size per arm after adjusting for the design effect)
m=1107 per study arm
Multiply by the two arms the total number of expectant mothers to be engaged in both arms will be 2214.
Therefore, a sample size of 2214 with 1107 expectant mothers per arm will be sufficient to detect a clinically important difference of 38.6% between groups in the mobile telephone communication intervention, using a two sided test of 80% power (β) and 5% of significance level (α) with 95% confidence interval.
Obtaining the Number of Clusters
The minimum number of units required to attain a 5% level of significance will be four per arm assuming normality for the cluster level responses and the use of non-parametric test, Mann–Whitney U-test 16-18. Therefore, the least number of expectant mothers a cluster can have is four.
Furthermore, researchers aver that with three units per arm, it is within the bounds of chance that the outcomes in the three treatment arms are all greater than the outcomes in the three control arms, but with four per arm, this is unlikely to happen by chance more than 1 in 20 times17. Therefore, the minimum number of clusters is four per arm (eight in total) for an unmatched design or six matched pairs for a matched design.
To Determine Number of Clusters Needed ( n_cluster )
n_cluster = Total number of participants in the two groups (/ fixed cluster size)
= 2241 / 80
=28.01 cluster~28 clusters
Therefore, the study will have a total of 28 clusters, 14 clusters being randomized to the intervention arm and 14 randomized into the control group.
Sampling Techniques
Sampling of Participants for Quantitative Data Collection
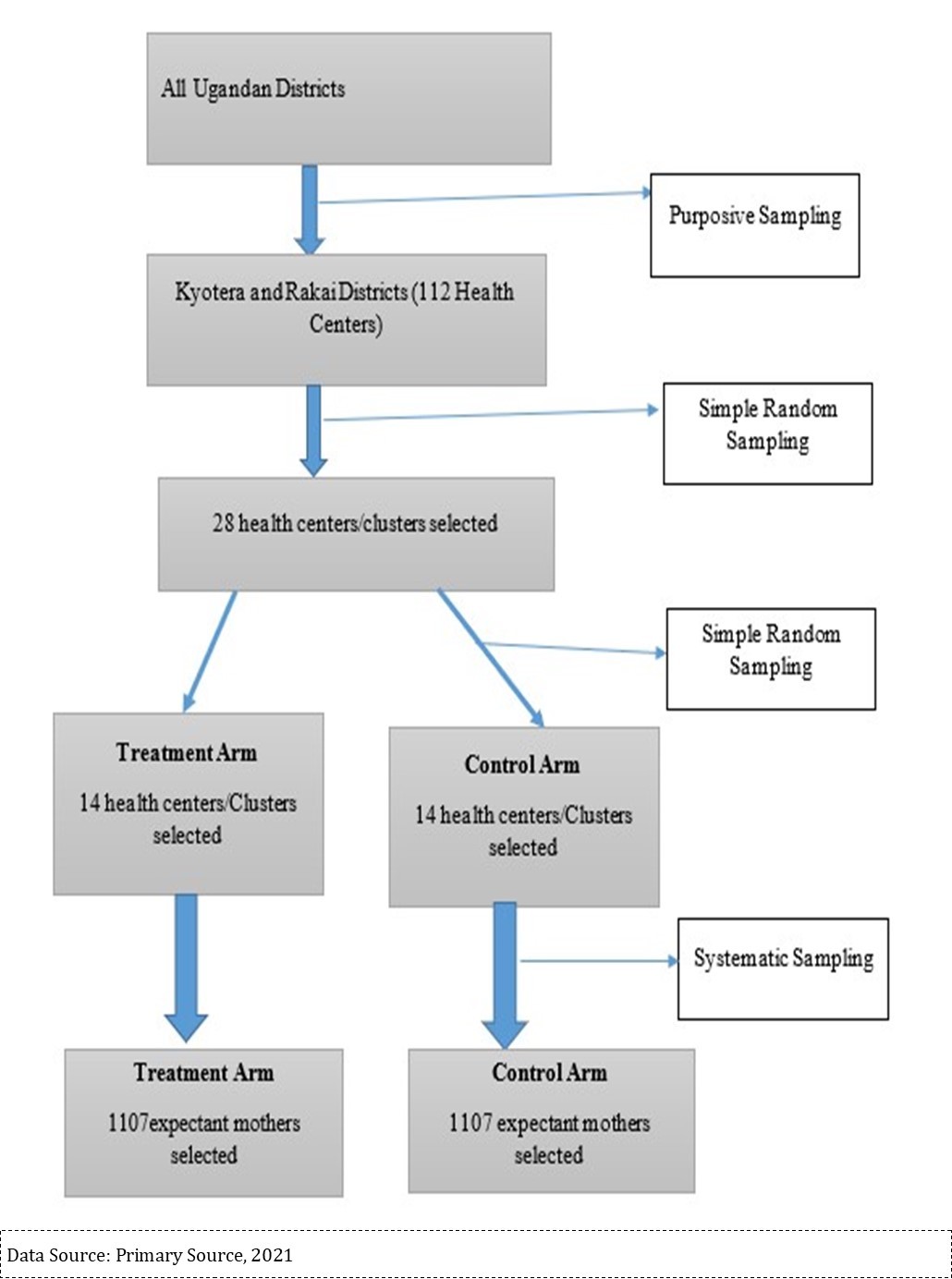
The study will apply the multi-stage sampling technique to select the study participants. With the multi stage sampling method, the study will be able to divide the population of expectant mothers into groups/clusters at different stages to ease data collection, management, and interpretation. The districts of Kyotera and Rakai are purposively sampled due to the low uptake of ANC services estimated at only 39%; which is below the desired national consumption of 47.5% 15. The gap in in the utilization of ANC services arises from the inadequate maternal health information that is availed to expectant mothers in the districts of Kyotera and Rakai13. Kyotera and Rakai Districts have a total of 112 registered medical facilities spread across the three counties of Kakuuto, Kooki and Kyotera20. In order to ensure that any baseline differences in group characteristics are purely as a result of chance rather than systematic bias, the cluster will be the unit of randomization in this study.
Cluster Sampling
Clusters of expectant mothers obtaining ANC services from selected health Centres who representative of the target population will be identified and included in the sample 22. Each health facility will be a cluster and it will be the sampling unit. The sampling frame will be comprised of all registered health facilities whose list will be obtained from the district health officers in the two districts. The facilities will be ranked based on the number of expectant mothers attending ANC at the different facilities. The 28 clusters (health Centres) with the highest ANC attendance will be prioritized in the study.
Random Sampling
After obtaining the 28 health centers from the register of health Centres, each will be allocated unique identification number that will be written on small pieces of paper and placed in a box. The random numbers will be written in such a way that 14 health centers will be allocated to the intervention arm (7 Kyotera and 7 Rakai district) and 14 allocated to the control arm (7 Kyotera and 7 Rakai district). This we be done to ensure that the allocation into the study arms is balanced across the two districts.
Other factors that will be considered for inclusion of a health facility into the study include;
a) Willingness to participate in the study by the in charge of the facility and the midwife.
b) Availability of ANC services.
c) Geographical location of the health centre randomly sampled
Systematic Sampling
Systematic sampling will be used to select the 2214 expectant mothers from the 28 clusters. A random expectant mother will be selected at the start and every ithmother who meets the eligibility criteria will be recruited into the study up to 80 expectant mothers per health facility. The sampling framework is displayed in Figure 1.
Recruitment of the Expectant Mothers
The research assistants will engage the in charges at the different health Centres to understand the ANC schedules and conduct a review of registers. After reviewing the registers, an engagement will be sought with the VHTs to conduct a community mobilization for the study participants. It is anticipated that when VHTs engage expectant mothers in the villages, the potential study participants will report to the selected health facilities for recruitment into the study. When the expectant mothers report to the health facilities, they will be received by the research assistants who will have a random start. Thereafter, the research assistant will discuss the study objectives with every ith expectant mother for recruitment into the study.
After explaining the study objectives to the potential study participant, the research assistant will administer the consent form and willingness to participate in the study will be affirmed by appending a signature or thumb print. On receiving a signed consent form, the expectant mother will provide baseline information to the research assistant obtained through completing the interviewer administered expectant mother questionnaire. This will lead to the allocation of the unique identification number for the expectant mother that will be used to follow up the mother during the study.
Where VHTs identify an expectant mother in the village who is eligible for recruitment and has not come to the health facility, the VHT will guide the research assistant to the potential participant. When the expectant mother signs a consent form, then they will be recruited into the study.
Description of the Intervention
Message Contents
In the intervention arm, mobile telephone phone-based text, recorded and voice messages comprising of information about the usefulness of maternal health services’ such as ANC, PNC and institutional delivery; and reminders of their next scheduled ANC appointment will be sent to expectant mothers and VHT’s hailing from villages served by health Centres in the intervention arm.
Particularly, every two weeks a text and voice message comprising of reminders for the next ANC visit, information about its importance of the first four ANC visits and expected date of delivery (EDD) will be sent to expectant mothers.
Scheduling of Expectant Mothers and Message Content
The international guidelines on maternal health supports the notion that the first ANC visit should be as early as possible in pregnancy, preferably in the first trimester; that is; within the first 12 weeks23. In a normal pregnancy, a minimum of four ANC visits is recommended23. Therefore, ANC follow-up visits will be scheduled based on GA with the first ANC visit preferably before 16 weeks of GA, otherwise at 16–24 weeks, the second ANC visit, between 24–28 weeks, the third ANC visit between 28–32 weeks and the fourth ANC visit 32–40 weeks. The last visit will be closely scheduled to the EDD to ensure that the appropriate guidance and healthcare are provided to reduce and manage any emergencies that may arise.
Based on the proposed enrollment framework for the expectant mothers for the study, any mother with a GA of 8 weeks will get first text and voice message. The message will have a reminder and information about the advantages for the first ANC visit. The same voice message will be continued every 2 weeks until the end of the time frame for the first ANC visit which is 24 weeks of GA. Therefore, an approximate total of twelve voice messages will be sent as reminders for the first ANC visit and along with the advantages.
Based on the time frame for the second ANC visit (24–28 weeks of GA), the 13th voice message from the initial messages will be a reminder for the second ANC visit and information about its advantages. In this time frame, in this case maximum of two voice messages will be sent. At the third stage a total of two text and voice messages will be sent with reminders for the third ANC visit and its advantages. This stage of messaging will thus start from the 15th voice message.
The fourth stage of voice messaging for ANC visit reminders and about its advantages will be started from the 17th voice message and this will consist of three parts (reminders for the fourth ANC visit, EDD and advantages of the fourth ANC and institutional delivery).
A maximum number of voice messages from the date of enrollment and until the 42nd week of GA will be 21 voice messages.
After the 21st voice message, the message will be changed to reminders for completion of the exit interview data instrument. Hence, the overall number of voice messages which will be sent for the intervention purpose will be twenty-two.
Message contents will be developed in English and then translated into Luganda. The messages will then be scripted to a female voice through a smart phone recording. Finally, these messages will be loaded on the mobile phone in voice message form to be sent regularly every 2 weeks at 9:00 a.m. to the intervention group.
Description of the Control Group
In the control group, expectant mothers will receive existing maternal health information that informs them about the advantages of maternal health care service use at the respective health centers. The expectant mothers will obtain information verbally from the midwives at the health centers, informing them about the available services and giving appointments for scheduled ANC visit.
No mobile text/ voice message will be sent to expectant mothers in this group. Base line data will be collected by VHT’s and research assistants from the expectant mothers who meet the eligibility criteria across the 19 Sub-Counties of Kyotera and Rakai Districts. The data to be collected will focus on the key components identified in the designed data collection instruments.
In the event that an expectant mother moves to another location that is not within the study area before the end of the study period, they will be registered as drop-outs irrespective of the study arm. The status of delivery will be tracked by VHT’s and research assistants in view of the fact that mothers have different gestation periods.
Following up Expectant Mothers
Intervention Arm
Health Centers randomized into the intervention arm and mothers enrolled into the study in these health Centres will be followed up by the VHTs only a monthly basis. This is in addition to the fortnightly maternal health messages (voice and text) reminders that will be sent to mobile telephones.
The VHTs will put emphasis on encouraging women who have received messages to go and receive ANC at the health facility as reminded. The VHT will be required to report those who have missed any ANC visits, had any complications and those who have changed location.
A midterm review of ANC registers at the health Centres to establish the number of times an expectant mother has utilized ANC services will be conducted by the research assistants.
Similarly, at the time of delivery, a mother will be required to complete an interviewer administered exit interview that will enrich the study with details of the 9months. This will be done by the research assistant. Where the delivery is done outside the health facility, the research assistant will be guided by the VHT to the home of the study participant to have the form completed.
Control Arm
Expectant mothers in the control arm will be monitored by VHTs and will be reminded that ANC services are available at the nearby health facility with no additional information. The VHTs will similarly be required to report those who have missed any ANC visit, had any complications and those who have changed location.
A midterm review of ANC registers at the health Centres to establish the number of times a study participant has utilized ANC services will be conducted by the research assistants.
Similarly, at the time of delivery, a mother will be required to complete an interviewer administered exit interview that will enrich the study with details of the 9 months ANC services utilization. This will be done by the research assistant. Where the delivery is done outside the health facility, the research assistant will be guided by the VHT to the home of the study participant to have the form completed.
Data Collection Methods
Quantitative data will be collected using the survey method at three intervals during the 12months. Expectant mothers will provide baseline data at the commencement of the study, at 6months data will be collected from ANC registers and at 12 months an interviewer administered questionnaire will be completed by expectant mothers. Qualitative data will be collected to enrich quantitative findings mainly using in-depth key informant interviews and focus group discussions once for the 12months period.
Data Collection Tools
Quantitative data will be collected using the interviewer-administered questionnaire. On the other hand, qualitative data will be collected using the Key Informant Interview guide and discussions using the Focus Group Discussion guides.
Participants
The study respondents to the interviewer administered questionnaires, key informant interviews and focus group discussions are categorized as shown in Table 1.
Table 1. Sample Frame Showing Categorization of Participants| Category of Participants | Target Population | Sample Size | Sampling Technique |
| Quantitative Sample Frame | |||
| Health Centres | 112 | 28 | Simple Random Sampling |
| Expectant mothers | 5589 | 2*1107=2214 | Systematic Sampling |
| VHTs | 117 | 28 | Simple Random Sampling |
| Total | 5818 | 2270 | |
| Qualitative Sample Frame | |||
| District Health Officers | 200 | 5-25 | Stratified sampling |
| Nurses | 112 | 5-25 | Purposive |
| Midwives/In charge HC | 112 | 5-25 | Purposive |
| District & Community Leaders | 70 | 5-25 | Purposive |
| Husbands to mothers | 800 | 5-25 | Convenience |
| VHT’s | 150 | 5-25 | Convenience/SRS |
| Total | 1444 | <=50 | |
Validation of Data Collection Instruments
The data collection instruments to be used in the study will be tested for face and content validity. This validation of instruments will ensure that the tools accurately measures what it aims to measure, regardless of the respondent. A valid data collection tool supports the collection of better quality data with high comparability and increased data credibility.
Data Analysis
Quantitative
Analysis will be done using aggregate cluster-level analysis; Regression analysis using individual expectant mother data with robust standard errors; Random-effects (Res) models using individual expectant mother data and; population averaged models using individual patient data with regression coefficients estimated using generalized estimating equations (GEEs). During the study, data exploration will be done to visualize the general features of the data then the key analysis will be conducted using SPSS version 20 at both cluster and individual level.
Descriptive Statistics
Summary statistics for the categorical ANC utilization outcome will be generated in form of means, proportions, frequencies and percentages depending on the nature of the data.
Measures of central tendency for both clusters and individuals such as frequencies, mean, medians and standard deviations will formulate the descriptive statistics that will be generated to describe the characteristics of the study population on sex, age, socio-economic, education level, distance from the health center and transport costs among others.
Inferential Statistics with Associations Inclination
The Chi-Square test and Pearson’s correlation product moment will have generated from the data to determine the association between mobile telephone services and ANC uptake among expectant mothers in Kyotera and Rakai Districts.
The paired t-test will be used to test whether the mean difference of the ANC utilization between the intervention and control groups is zero or not.
Inferential Statistics with Effect Inclination
On the other hand of inferential statistics, a general logistic regression model will be fitted to the data to the assess the impact of the intervention i.e. mobile telephone services on the ANC uptake. In order to identify independent factors that influence the uptake of ANC services among expectant mothers in Kyotera and Rakai Districts, a multiple logistic regression model will be fitted to data.
A path analysis will be conducted to examine the comparative strength of direct and indirect relationships among variables using the Structural Equation Modelling (SEM). With the use of SEM the study will be able to measure and analyze the relationships of observed and latent variables
Qualitative Data Analysis
Content Analysis
The data obtained from FGD and key- informant interviews regarding the attitudes and perceptions of expectant mothers about the ANC uptake in Kyotera and Rakai Districts will require coding and categorization into themes. Therefore, content analysis will formulate the basis for the engagement of other qualitative analysis methods.
Thematic Analysis
The study will deploy a thematic analysis to display and classify data from the two study arms based on similarities and differences25. The use of thematic analysis will provide an opportunity to understand the criticality of any issues regarding ANC uptake among expectant mothers 26.
Studies emphasize that apart from counting explicit phrases and words, the thematic analysis pays due attention to ascertaining and describing both explicit and implicit proposal therein 27. The coding generated for the different themes and ideas is the aligned to the raw data as summary markers for advanced analysis which may include graphical displays of code patterns and relationships, drawing comparisons on the relative frequencies of themes and ideas for a give data file and obtaining of code co-occurrence.
Results and Discussion
Expected Results
The study is expected to rise awareness about the availability of ANC services among expectant mothers in the districts of Kyotera, increase the utilization of ANC services given the scheduled reminder text and voices messages; and overall behavioral change among expectant mothers.
Discussion
Improvement of maternal health is a priority focus area on the sustainable development goals agenda. However, indepth evidence about the barriers to access and utilization of maternal health services specifically among the rural illiterate pregnant women remains lacking 28. Collaborations with mobile telecommunications companies is among the key enlisted strategies towards the improvement of maternal health2. A number of studies focusing on mhealth solutions geared towards increasing adherence to utilization of maternal health services have been conducted in Sub-Saharan Africa (SSA.) In recent studies, text messages have been used to remind expectant mothers about scheduled visits29,33yet the current study will deploy both text and voice messages to account for illiterate mothers who may not be able to read text messages. Furthermore, expectant mothers have been recruited from health facilities34,35yet the current study will engage VHT’s in the mobilization of expectant mothers for recruitment into the study. Therefore, the mobile telephone communication voice and text based intervention should generate strong evidence on ANC utilization in rural settings with lower literacy levels literacy, which may be generalized to poorly resourced setting in Africa and world at large.
Conclusion
The usage of mobile telephone communication interventions to provide maternal health information to expectant mothers in Kyotera and Rakai Districts will provide critical information for research regarding the consumption levels of different antenatal care services among expectant mothers in Kyotera and Rakai Districts, other rural districts in Uganda and less resourced countries around the world. The study will raise awareness of expectant mothers in Kyotera and Rakai Districts about the availability of antenatal care services. This will in turn increase the utilization of ANC services, having deliveries assisted by professional health workers which will reduce maternal morbidity and mortality.
Study findings will guide health service providers in Kyotera and Rakai Districts in determining ways of enhancing utilization of ANC services. This will inform policy formulation at district, regional and national level for the achievement of the sustainable development goal target of below 70deaths per 100000 by 2030.
Abbreviations
ANC-Ante Natal Care
MMR-Maternal Mortality Ratio
SDG-Sustainable Development Goals
WHO- World Health Organization
AHSPR-Annual Health Sector Performance Report
ITT- Intent To Treat, VHT-Village Health Teams
TBA-Traditional Birth Attendants.
References
- 1.Travaline J M, Ruchinskas R, D'Alonzo GE Jr. (2005) Patient-physician communication: why and how. , J Am Osteopath Assoc. Jan. PMID 13-18.
- 3. (2017) World Health Organization (2017). Maternal mortality: Levels and trends o,. World Health Organization:. , CC BY-NC-SA 3, 182-187.
- 4.Creanga A A.Maternal mortality in the United States: a review of contemporary data and their limitations. [PubMed] [Google Scholar] , ClinObstetGynecol 61(2), 296-306.
- 5.C R McNellan, Dansereau E, Wallace, M C G. (2019) Antenatal care as ameans to increase participation in the continuum of maternal and child healthcare: an analysis of the poorest regions of four Mesoamérican countries. , BMC Pregnancy Childbirth 19, 2019-10.
- 6. (2016) World Health Organization. Health statistics and information systems: maternal mortality_ ratio.
- 7.Agho K E, Ezeh O K, Ogbob F A, Enoma A I, Greeno C R. (2018) Factors associated with inadequate receipt of components and use of antenatal care services in Nigeria: a population-based study PMID. 65-76.
- 9.Kawungeezi P, AkiiBua D, Aleni C, Chitayi M, Niwaha A et al. (2015) Attendance and Utilization of Antenatal Care Services: Multi-Center Study in upcountry areas of Uganda. 36, 42-46.
- 10.Ministry ofHealth Uganda. Annual Health Sector. Performance Report 2016/17. Kampala-Uganda. AHSPR. (2017).39-40
- 13.Ministry ofHealth Uganda. Annual Health Sector Performance Report 2019/2020. Kampala-Uganda. AHSPR.2020 23-27.
- 14.Musiimenta A, Tumuhimbise W, Pinkwart N, Katusiime J, Mugyenyi G et al. (2021) A mobile phone-based multimedia intervention to support maternal health is acceptable and feasible among illiterate pregnant women in Uganda: Qualitative findings from a pilot randomized controlled trial. DIGITAL HEALTH.;7 .
- 15.Amooti Kaguna B, Nuwaha. Mbarara University of Science and Technology, Department of Community Health. Soc Sci Med (2000) Factors Influencing Choice of Delivery Sites in Rakai Districts ofUganda. 34-36.
- 16.R J Hayes, Bennett S. (1999) sample size calculation for cluster randomized trials. , Int. J. Epidemiol
- 17.M J Campbell, S J Walters. (2014) How to Design, Analyze and Report Cluster Randomized Trials in Medicine and Health Related Research;. , Ltd.: Chichester, UK
- 19.Aparasu R. (2011) Research Methods for Pharmaceutical Practices and Policy; Pharmaceutical Press:. , Maryland Heights, MO, USA
- 20. (2015) Rakai District Local Government. Five Year District Development Plan for2015/2016-2019/2020.
- 21. (2017) Uganda Bureau of Statistics. The National Population and Housing Census. Area Specific Profile Series , Kampala, Uganda .
- 22.Rutterford C, Copas A, Eldridge S. (2015) Methods for sample size determination in cluster randomized trials.
- 23.S L Jackson. (2011) . Research Methods and Statistics: A Critical Approach, 4th ed.; Cengage Learning: , Boston, MA, USA .
- 24. (2002) World Health Organization WHO Antenatal Care Randomized Trial. Manual for implementation of new model. Department of Reproductive Health and Research. , Geneva, Switzerland
- 27.Namey E, Guest G, Thairu L, Johnson L. (2008) Data Reduction Techniques for Large Qualitative Data Sets. In: Handbook for team-based qualitative research. , Rowman Altamira
- 28.Tumuhimbise W, Esther C, Ayebaza S, Katusiime J, Mugyenyi G et al. (2020) Maternal health-related barriers and the potentials of mobile health technologies.
- 29.Lund S.Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomized controlled trial. , BJOG 119(10), 1256-64.
- 30.Mathauer I. (2006) Imhoff I. Health worker motivation in Africa: the role of nonfinancial incentives and human resource management tools. Hum Resour Health.
- 32.Mahmud N, Rodriguez J, Nesbit J.A text message-based intervention to bridge the healthcare communication gap in the rural developing world. , Technol Health Care 18.
- 33.Lee S H. (2013) Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: systematic review and meta-analysis. , J Glob 6(1), 010401.