Self-Efficacy and Smoking Cessation: A Mixed Method Study among Adult Smokers in Fiji
Abstract
A mixed‑methods study examines self‑efficacy in smoking cessation among Fijian adults. It outlines qualitative themes and quantitative associations to guide tailored interventions.
Author Contributions
Academic Editor: Qiang Cheng, Biomedical Informatics Institute, and Computer Science Department.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2023 Masoud Mohammadnezhad, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Cigarette smoking is one of the modifiable risk factors for non-communicable diseases (NCDs) and is currently a major leading cause of preventable death worldwide 1, 2. It is the main risk factor for lung cancer and a major cause of cardiovascular morbidity and mortality worldwide 3, 4. It was estimated that 8 million people would die each year by 2030 if the current trend of smoking consumption remained unaddressed 5.
Studies have estimated that 1 in every 10 deaths in the world are caused by smoking 6; it is the leading cause of preventable deaths in the US 7. Studies have also found that over 80% of the world’s smokers lives in low and middle-income countries 8, 9. Some developed countries around the world have seen the decline of smoking prevalence among their adult population and this is especially true for the US 20.9% in 2005 to 16.8% in 2014, western Australia 27% in 1998 to 15% daily smokers in 2013, and Hong Kong 18.8% in 1998 to 10.5% daily smokers in 201510. The concern with high smoking prevalence in lower socioeconomic populations is that they usually carry a greater burden of smoking related illness 11. Furthermore, researchers have found high smoking prevalence among populations who had divorced or separated from their partners, however, it also noted that smoking prevalence varies by intersection of marital status, race and ethnicity 12. In Fiji, the latest statistics about tobacco consumption available from the 2002 and 2011 STEP Survey have reported the trend of significant decline of smoking prevalence in both sexes and ethnicities. The figures stated it was 63% in 2002 compared to 52% in 2011 for I-taukei men; 54% in 2002 to 42.3% in 2011 for Indian men; 29.5% in 2002 to 24.2% in 2011 for I-taukei women; and 4.7% in 2002 to 2.3% in 2011 for Indian women 13.
As has been noted, smoking is a major cause of premature deaths worldwide and it is because of increasing risk of metabolic syndrome and diabetes which ultimately leads to cardiovascular diseases 14. It also has a detrimental effect on mental health such as schizophrenia and depression 2. Therefore, smoking cessation is especially important because it can help reduce the risk of developing cardiovascular diseases and other diseases that are associated with it 15.
One of the most important factors that can help support smoking cessation is making sure that the self-efficacy of people is higher and exposure to cigarette smoke is avoided 16. Researchers revealed that factors that can increase self-efficacy among smokers to quit smoking include motivation to quit, as well as a strong will power to quit 17. Some of the strategies to motivate smokers to attempt quitting smoking include taking advantage of teachable moments post heart attack; psychoeducation, and fear arousal via presentation of negative smoking consequences 18. It is also important to note that there are other factors such as fear of withdrawal symptoms that can also contribute to low self-efficacy 19, 20.
Another important factor to consider for a successful smoking cessation program is the need to look at determinants of quitting 21. Some determinants of smoking cessation included health related problems, inaccessibility of a smoking zone, pressure from non-smoking spouse and not living with a smoker 22, 23. On the other hand, personal factors and environmental factors such as poor knowledge of the dangers of secondhand smoke, addiction to nicotine and protective measures and the lack of smoking laws to ban smoking have been found to be the most important barriers towards quitting smoking 16, 22. In terms of the role of family, studies have found that some of the barriers towards abstinence from smoking, especially among adolescent smokers, includes peer pressure and weak parental control 24. Furthermore, researchers have also highlighted that high nicotine dependence and having a low level of education are also associated with low smoking cessation rates 25.
To the best of our knowledge, there has not been any study conducted in Fiji about smoking therefore, this study aimed to assess self-efficacy of smokers and to explore factors affecting confidence and quitting smoking among current adult smokers in Suva, Fiji. This information is important as it can help inform the design of an evidence-based smoking cessation program in Fiji.
Materials and Methods
Study design and setting
A mixed method study design was carried out to assess smokers’ self-efficacy, as well as their perception on factors affecting their confidence and smoking cessation in Suva, Fiji between 1st May to 31st July 2020. Three randomly selected healthcare centers, among seven available healthcare centers in Suva, were chosen based on geographical distribution to conduct this study including: Nuffield, Samabula, and Valelevu health centers.
Study sample
We included current smokers who were over 18 years and were attended one of the three selected healthcare centers during the study period. Those who had mental instability to answer questions or were not willing to participate in the study were excluded.
For the quantitative study, the sample size was calculated based on the sample population proportion formula for one month that applied a 50% prevalence of self-efficacy, 95% confidence interval (95% CI), and 5% margin error. It was estimated that about 150 smokers per month attended the selected healthcare centers, therefore, 450 smokers were considered as study sample. By adding a 10% non-respondent rate, in total 495 smokers were selected as a sample. For the qualitative study, those who participated in the quantitative study were chosen purposively and in-depth interview was continued to reach data saturation at 35 smokers’ attendance.
Data collection tools
For quantitative study, a self-administered questionnaire was used to collect data. The questionnaire was developed based on the literature review and other questionnaires that have been used in previous similar studies. The questionnaire had four sections including background information (5 questions), smoking cessation (4 questions), self-efficacy to quit smoking (9 questions), and stage of change (5 questions) 26. A shortened form of the Smoking Abstinence Self-efficacy Questionnaire (SASEQ) 27 was used to measure self-efficacy with 5 Likert scale answers ranging from “not at all”, “not very”, “moderately, “very” and “extremely”. They were scored from 1 to 5 and the total score of <27 was considered as “low level”, 27-36 as “medium level” and ≥37 as “high level” of self-efficacy.
To do face validity, the questionnaire was tested in a pilot study before being used in the main study. Ten smokers who met the study criteria were asked to read the questionnaire and provide their feedback. The content of the questionnaire was tested by three experts in the field of smoking and their comments were used to modify the questionnaire. After the changes were made, the final questionnaire was translated to Fijian and Indian languages by bilingual translators. Reliability of the questionnaire was measured through test-retest reliability and the questionnaire was given to 30 participants in two stages with a final Cronbach alpha of 0.85.
For the qualitative study, a semi-structured questionnaire was used that had two sections to collect participants’ demographic information, as well as 7 open-ended questions to understand participants’ perception on smoking and factors affecting their self-efficacy and smoking cessation.
Study procedures
One week before starting this study, the information related to this study was provided to all potential participants in three healthcare centers.Those who were interested in participating in this study were given an information sheet and a written consent form in three languages (Fijian, English and Fiji Hindi) to read and sign before collecting the data. They were asked to fill out the questionnaire in their preferred language (Fijian, English and Fiji Hindi) while they were waiting in the main waiting hall. For those who were not able to complete the questionnaire at the same time, a prepaid envelope was provided and they were asked to complete the questionnaire within one week and return to the researcher. Assistance was provided to those who were not able to read or fill the questionnaire by a bilingual research assistance. For the qualitative study, the same procedure was done, and in-depth interviews were conducted by a trained research assistant in a private room after scheduling a meeting with the participants in one of the selected healthcare centers. The interview was recorded by a digital recorder and each interview took about 30-40 minutes. The recorded interview and transcribed scripts were accessible to the principle investigator which are kept in a computer with password protection. They will be discarded after three years.
Data management and analysis
Descriptive analysis was done after cleaning the data using Statistical Package for the Social Sciences (SPSS) version 24. The results were presented in the form of frequency, percentage, mean and Standard Deviation (SD). For the qualitative study, thematic analysis was used manually to find the common themes. To do that, transcription was done by two independent researchers and codes were identified after reading and re-reading transcriptions. Similar codes that had the same meaning were combined to make sub-themes and finally similar sub-themes were combined to identify common themes.
Ethical considerations
Ethical approval was obtained from the College Health Research Ethics Committee (CHREC) and Fiji National Health Research and Ethics Review Committee (FNHRERC) with ID#2019.24.C.D. In addition, the permissions were collected from the doctor in charge of each of the three selected healthcare centers.
Results
Quantitative Findings
Overall, 464 smokers participated in this study with the respondent rate of 93.7%.
General characteristic of participants
Table 1 illustrates general characteristics of participants. The mean age of participants was 32.7 (SD=12.1) with the majority (46.8%) in the age group of 20-29. More than two thirds of them (74.1%) were male. Majority of participants (72.6%) were I-taukei with secondary and tertiary education (43.5% and 48.5%, respectively) and annual income of $8,000-15,000 FJD (26.5%).
Table 1. General characteristics of study participants (n= 464)| Variables | Frequency | Percentage |
| Age Group | ||
| <20 | 26 | 5.6 |
| 20-29 | 217 | 46.8 |
| 30-39 | 114 | 24.6 |
| 40-49 | 57 | 12.3 |
| ≥50 | 50 | 10.8 |
| Gender | ||
| Male | 344 | 74.1 |
| Female | 120 | 25.9 |
| Ethnicity | ||
| I-taukei | 337 | 72.6 |
| Indian | 111 | 23.9 |
| Others | 16 | 2.3 |
| Educational level | ||
| No formal education | 5 | 1.1 |
| Primary | 32 | 6.9 |
| Secondary | 202 | 43.5 |
| Tertiary/Higher | 225 | 48.5 |
| Annual Family income (FJD*) | ||
| < 8000 | 123 | 26.5 |
| 8000 – 15000 | 190 | 40.9 |
| 15000 – 25000 | 97 | 20.9 |
| 25000 – 35000 | 32 | 6.9 |
| > 35000 | 22 | 4.7 |
Quit smoking characteristics
When they were asked, “Have you tried to quit or reduce the number of cigarettes,” 86.2% of participants answered yes. As Figure 1 shows, majority of participants mentioned that they tried to quit smoking by own (86.6%) while only 8.9% mentioned they were advised by other health care professionals to quit smoking. Six-point five percent of them quit smoking by attending stop smoking group/class.
Figure 1.Distribution of participants based on smoking cessation methods (n=35)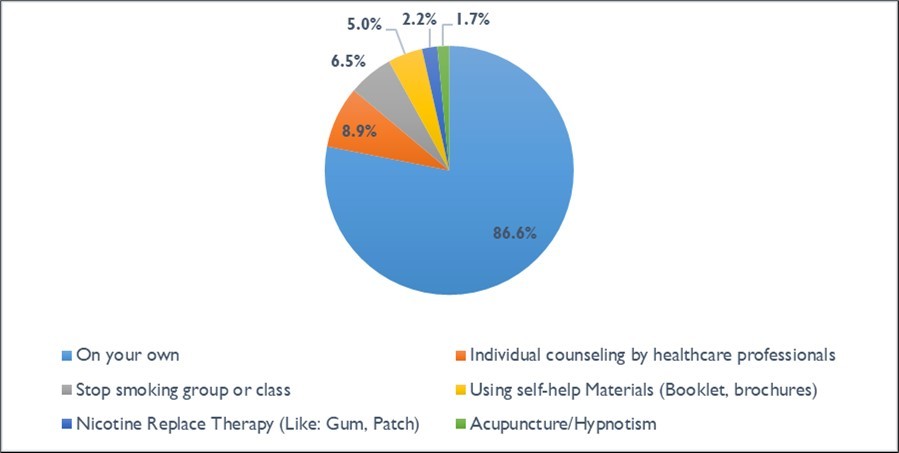
Table 2 shows other characteristics of smoking cessation among participants. More than two thirds of participants (72.8%) quit smoking because they wanted to promote their health, followed by healthcare workers advice (50.9%), saving money (28.9%) and their appearance (24.1%). Only 12.5% of them quit smoking due to their relative’s advice. The results also showed that, the main barrier to quit smoking was smoking friends/colleagues (39.9%), followed by physiological craving (31.5%) and withdrawal symptoms (30.2%), while 15.1% of them stopped smoking due to gaining weight. One third of participants (34.7%) believe their spouse can help them to quit smoking, followed by friends (28.8%) and healthcare workers (25.1%), while 11.6% mentioned their colleagues can help them better to quit smoking.
Table 2. Characteristics of smoking cessation among participants (n=464)| Variables | Frequency (n) | Percentage (%) |
| Reasons for smoking cessation | ||
| To improve my health | 338 | 72.8 |
| For my appearance | 112 | 24.1 |
| Persuaded by friends | 72 | 15.5 |
| To save money | 134 | 28.9 |
| For my family’s health | 73 | 15.7 |
| Persuaded by relatives | 58 | 12.5 |
| Advised by healthcare professionals | 236 | 50.9 |
| Barriers of smoking cessation | ||
| Psychological craving | 146 | 31.5 |
| Habit | 127 | 27.4 |
| Withdrawal symptoms (headache, dizziness…) | 140 | 30.2 |
| Smoking family member | 82 | 17.7 |
| Gained weight | 71 | 15.1 |
| Smoking friends/colleagues | 185 | 39.9 |
| Best supporter to quit smoking | ||
| Spouse | 161 | 34.7 |
| Sibling(s) | 103 | 22.1 |
| Other relative(s) | 113 | 24.7 |
| Health care worker(s) | 117 | 25.1 |
| Friend(S) | 134 | 28.8 |
| Child(ren) | 56 | 12 |
| Co-worker(s) | 54 | 11.6 |
| None | 62 | 13.3 |
Smokers’ stage of change
Table 3 demonstrates the stage of smoking according to Stage of Change Model (SCM). The results show that majority of participants (87.1%) were thinking of quitting smoking. It also illustrates that 27.6% of participants were at the stage of “Pre-contemplation” (they had no intention to quit smoking in the next 6 months). More than one third (37.7%) of them were at the stage of “Contemplation” (seriously consider quitting smoking in the next 6 months), while 16.6% of participants were at the stage of “Preparation” (decided to quit smoking in the next 30 days) and 4.95% of them were at the stage of ‘Action” (no smoking in the last 6 months). A small number of participants (2.4%) were at the stage of “Maintenance” (no smoking for more than 6 months).
Table 3. Frequency of participants in terms of stage of smoking cessation (n=464)| Frequency | Percentage | |
| Are you thinking of quitting smoking? | ||
| Yes | 404 | 87.1 |
| No | 60 | 12.9 |
| Which of the following statements describes the best your current situation? | ||
| I smoke and I have NO intention to quit smoking in the next 6 months | 128 | 27.6 |
| I smoke, but I seriously consider quitting smoking in the next 6 months | 175 | 37.7 |
| I smoke, but I have decided to quit smoking in the next 30 days | 77 | 16.6 |
| I am an ex-smoker, I quit smoking LESS than 6 months ago | 23 | 4.95 |
| I am an ex-smoker, I quit smoking MORE than 6 months ago | 11 | 2.4 |
Self-efficacy results
The mean of self-efficacy score was 27.7 (SD=8.5). Majority of participants (43.1%) had low self-efficacy to quit smoking (<27), 41.2% of them had medium level of self-efficacy to quit smoking (27-36) and 15.7% had high level of self-efficacy to quit smoking (36-45).
Qualitative Findings
Overall, 35 smokers participated in in-depth interviews. General characteristics of participants are presented in Table 4. The results reveal that majority of participants (48.6%) were in the age group of 18-24. They were mostly male (57.1%), I-taukei (77.1%) and Fijian of Indian Descent (20.9%), single (54.3%), with tertiary education (68.6%) and were unemployed (62.9%).
Table 4. General characteristics of study participants (n=35)| Frequency | Percentage | |
| Age | ||
| 18 - 24 | 17 | 48.57 |
| 25 – 29 | 6 | 17.14 |
| 30 – 34 | 6 | 17.14 |
| 35 and over | 6 | 17.14 |
| Gender | ||
| Male | 20 | 57.14 |
| Female | 15 | 42.86 |
| Ethnicity | ||
| I-taukei | 28 | 77.14 |
| Fijian of Indian Descent | 7 | 20.9 |
| Marital Status | ||
| Married | 12 | 34.29 |
| Single | 19 | 54.29 |
| Separated | 3 | 8.57 |
| Divorced | 1 | 2.86 |
| Education | ||
| Tertiary | 24 | 68.57 |
| Secondary | 11 | 31.43 |
| Primary | 0 | 0 |
| Employment Status | ||
| Unemployed | 22 | 62.86 |
| Employed | 13 | 37.14 |
The content analysis revealed the findings of two themes, one is the determinants of self-efficacy and second is factors affecting smoking cessation, as presented below.
Theme 1: Determinants of self-efficacy
The qualitative study identified some of the factors that assisted in motivating smokers to have confidence in quitting smoking including: health related factors, the desire or the interest to improve physical appearance, financial constraints and the intention to cut personal expenditure to save money. For instance, losing weight or having dirty face due to smoking were reasons to motivate them to quit smoking.
“yeah so I lost weight and my face ahhhh was not that much clean to me so I needed to quit smoking” (P5; 21 Male; I-taukei)
Gaining weight and improving physical appearance motivated smokers to quit smoking. A participant mentioned,
“Yes! I think it will help us to gain some weight as I will eat well, and our physical appearance will improve too”. (P18; 18 Male; I-taukei)
Another participant said,
“Yes, in terms of saving money, it will be useful for me. Well, money is just part of it but the health, which cannot be bought by money, right? So that’s a big benefit”. (P27; 32 Male; Fijian of Indian Descent)
Theme 2: Factors affecting smoking cessation
Close family members such as a mother and/or father can play an important role in encouraging smokers to quit smoking and reinforcing of a smoke-free home.
“If I quit smoking, for sure my mum will be happy um…..I may not really impress my other friends who smoke with me but at least I know that I have impressed my mum because she has always told me that I have to take care of my life and not follow my father as my father usually tell me to do what I wanted to do in my life”. (P34; 24 Male; I-taukei)
Another participant stated,
“Family! For the whole two weeks I stayed with my family and I had no other option, like um… I just had to not smoke at all. You see the environment was different as well and there is no need for me to smoke there” (P32; 24 Female; Fijian of Indian Descent)
Few of the study participants also stated that their addiction to smoking is what makes it harder for them to quit smoking.
“Um…… I think like I said it’s out of negligence...umm...as I have mentioned earlier that I`m more like an addicted smoker so leaving at this point in time would really a hard thing to do”. (P34; 24 Male; I-taukei)
Study participants also mentioned that having to live in an environment where everybody is smoking is also a factor that affects their confidence to quit smoking.
“my friend…yes we are all smokers….my other family members, cousins who are smokers…who will just come by…and say I bought you one packet…here semi your packet …… um …. your share of grog….and all …. Oh man I will just start smoking again…. hahaha”. (P7; 25 Male; I-taukei)
Most of the participants had mentioned that they needed guidance and assistance when they are motivated enough to quit smoking.
“Uhmm actually a good company to guide me through because I know what are the damages. Uhm… probably I cannot do it alone. That`s what I feel, I cannot do it alone.” “Probably, I haven’t heard of any counsellor to help in this kind of thing as we have seen in movies that abroad they have smoking counsellor, they got alcoholic counsellor but in here, there is nothing as such”. (P27; 32 Male; Fijian of Indian Descent)
Another participant mentioned,
“umm.. because when I drink grog that is why I wanted to start again. Also, roaming around with my friends while they are smoking, I can smell it and so I wanted to start again”. (P20; 25 Female; Rotuman)
Most participants stated that smoking helps them to establish friendships and be part of a group or circle of friends.
“Aahhmm just seeing my peers drinking and smoking I just said to myself I want to be like them too, so that I don’t feel left out, yeah.” (P4; 43 Male; I-taukei)
Another participant stated,
“Ah… back then, yeah, yes because mainly all of the, all of my friends were smoking. I was the only one, I was the odd one. So in order for me to… to be like them, so to join the crowd, I had to… to do it, to smoke.” (P6; 23 Male; I-taukei)
Most participants mentioned that the lack of willpower to say no to the offer of smoking from friends is the main barrier to quitting.
“…if they like light a cigarette in front of me, I’m obviously gonna smoke with them as well because I have this issue on um…. like self-control. Okay, yes that’s something that I lack, self-control. The willpower to say no, it's very weak…” (P30; 32 Female; I-taukei)
Discussion
Smoking is no doubt a major public health problem as it is the leading cause of preventable death 2. Henceforth, critical information is needed to successfully address smoking prevalence and improve smoking cessation programmes. Of vital information that needs to be explored is the factors affecting self-efficacy and quitting for current smokers. This section discusses these factors, considering the findings from this study and from other studies as well.
The results of our findings suggested that most smokers in this study would want to try to quit smoking by their own, and family members and health professionals, especially doctors, can play a vital role in encouraging them to do so. These findings are consistent with findings from other studies stating that smokers will successfully quit smoking if they are motivated enough, especially during teachable moments during and post illness and financial hardship moments 18, 28, 29. Unfortunately, findings from the quantitative study found that majority of the study participants mentioned that they were not advised by their doctor to quit smoking when they visited the healthcare facilities. This is consistent with the findings from other studies and it could be reasoned to the, “stress of diagnosis, time constraints, inadequate resources and lack of connection between smoking, cancer and health, beliefs among health professionals that someone else should deliver intensive behavioural support” 30, 31, 32. However, most participants in this study said they received more advice from their family members to quit smoking. This could be attributed to the fact that most of the smokers in this study are married and have 5-6 household members, which gives them many chances to receive advice from these family members. It could also be due to the fact that most of these smokers are aged 20-29 years old and their parents would still be alive to be advising them about making wise decisions in life. Studies have shown that having the advice from family members such as parents and spouse, is an effective way to motivate people to contemplate quitting smoking 33, 34. Further, findings from the qualitative study also reported the same issue with most of the study participants stating that they are not aware of any doctors or counsellors available to provide support to those who are willing to quit. This supports the influence of family support reinforcing behavioral change 35. The qualitative findings also found that the reasons behind smokers trying to quit smoking by their own include other factors such as having a strong interest to promote their own health and are experiencing financial constraints. Nevertheless, the lack of commitment from health professionals to advise current smokers to quit smoking could be a critical reason to the low self-efficacy of quitting smoking among current smokers as studies have suggested that smokers who intend to quit smoking need support over the course of smoking cessation 32, 36. Financial constraints could be one of the more important triggers that motivate study participants to quit smoking since we have noted from our quantitative findings that majority of them had a household income of $8,000 - $15,000 FJD per year, live in urban areas, are married and most had 5 to 6 household members. This finding supports the results of other studies stating that socioeconomic status is significantly associated with the ability to quit smoking 37, 38. In this study most of the study participants are seriously intending to quit smoking, and the fact that more than two thirds of the study participants were thinking of quitting smoking would confirm this. It is inconsistent with the findings from other studies that showed smokers have low levels of intention to quit, primarily because smoking is deeply integrated into their social norms 39, 40.
The findings of this study also revealed that majority of the smokers who quit the last time reasoned their cessation failed mostly by strong influence from smoking friends and psychological cravings. This is a crucial finding as it indicates that smokers have a low self-efficacy to quit smoking and the self-efficacy results confirmed this, noting that majority of the smokers had a low self-efficacy to quit smoking. These findings are consistent with findings from other studies, noting that smoking family members and friends are the main barriers to quit smoking, while addiction to smoking or nicotine dependence makes it an important part of life which is hard to get rid of 41, 42, 43, 44. The findings from the qualitative study reaffirm this revelation as most study participants also highlighted that smoking friends is the main barrier to successfully quit smoking while, and as well as, the lack of will power to refuse a cigarette when it is offered by smoking friends. This is similar to the findings from other studies 45, 46.
In terms of stages of change model, this study found that less than half of the study participants were at the stage of pre contemplation and contemplation while very few of them were at the stage of preparation, action and maintenance 47. The lack of intention and planning to quit smoking could be attributed to the strong influences of friends’ smoking, psychological cravings for smoking among current smokers, loss of a way to handle stress and perception that smoking helps establish friendship with other smokers, as was found in both the quantitative and qualitative part of the study 43, 48. Other studies have also found that smokers do not intend to quit smoking mainly because of addiction or high nicotine dependence, and lack of information and perceived availability of support to quitting 49, 50. Our qualitative finding also noted that most participants lack the will power to say no when a cigarette is being offered by a smoking friend. It is understandable that very few of the study participants are at the stage of preparation, action and maintenance of quitting smoking because this study only recruited current smokers, and also less than half of the study participants are in the contemplation stage of quitting.
Limitations
Although, this mixed method study is the first study conducted among adult smokers in Fiji, there are few limitations.The results of the quantitative cross-sectional study cannot be generalized to all smokers in Fiji. It also used a self-administered questionnaire to collect data that relied on participants answering at the time of collecting data. Their answers may change in another situation. The qualitative study was only conducted among smokers. Conducting interviews among healthcare workers could provide more information about strategies to help smokers. This study was conducted in the Covid-19 situation that has affected the time and the procedure of study.
Conclusions
The results of this study showed a low level of confidence among smokers. Considering the results of this study and factors highlighted in both qualitative and quantitative study can help decision makers to developed smoking preventive strategies. Using theories and models that focus of changing behaviors, such as Health Belief Model (HBM), Transtheoretical Model (TTM) and Stage of change, can help smokers to quit smoking. Family support and promoting community knowledge about smoking and its harms can reduce smoking among smokers. School based education should be a priority to prevent smoking among Fijians.
Authors’ contributions
MM: Conceptualization, methodology, data curation, writing manuscript. MK: writing manuscript. SK: analyzed the data. LM: data collection. TM: edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This project was funded by the Fiji National University grant.
Availability of data and materials
The data will be available from the corresponding author on reasonable request.
Institutional Review Board Statement
Ethical approval was obtained from the Fiji National University (FNU), College Health Research Ethics Committee (CHREC)- ID: 010.19. Written informed consent was obtained from the participants. We also confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Acknowledgements
We acknowledge the Fiji National University for granting this project. We also appreciate all the study participants.
References
- 1.Grech L B. (2020) Modifiable risk factors for poor health outcomes in multiple sclerosis: the urgent need for research to maximise smoking cessation success. Mult Scler. 26, 266-71.
- 2.Wootton R, Richmond R, Stuijfzand B, Lawn R, Sallis H et al. (2019) Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychol Med. 50-14.
- 3.Rezk-Hanna M, Benowitz N L. (2018) Cardiovascular effects of hookah smoking: potential implications for cardiovascular risk. Nicotine Tob Res. 21(9), 1151-1161.
- 4.Biondi‐Zoccai G, Sciarretta S, Bullen C, Nocella C, Violi F et al.Acute Effects of Heat‐Not‐Burn, Electronic Vaping, and Traditional Tobacco Combustion Cigarettes: The Sapienza University of Rome‐Vascular Assessment of Proatherosclerotic Effects of Smoking (SUR‐VAPES) 2 Randomized Trial. , J Am Heart Assoc 8(6).
- 5.Demaio A R, Nehme J, Otgontuya D, Meyrowitsch D W, Enkhtuya P. (2014) Tobacco smoking in Mongolia: findings of a national knowledge, attitudes and practices study. BMC Public Health. 14-213.
- 6.Ghenadenik A E, Gauvin L, Frohlich K L.Residential environments and smoking behaviour patterns among young adults: a prospective study using data from the Interdisciplinary Study of Inequalities in Smoking cohort. Prev Med. 2019, 48-54.
- 7.Koslovsky M, Hébert E, Swartz M, Chan W, Leon-Novelo L et al. (2018) The Time-Varying Relations Between Risk Factors and Smoking Before and After a Quit Attempt. Nicotine Tob Res. 20(10), 1231-1236.
- 8.Caleyachetty R, Tait C A, Kengne A P.Tobacco use in pregnant women: analysis of data from Demographic and Health Surveys from 54 low-income and middle-income countries. Lancet Glob Health 2014;2:e513–20. 10-1016.
- 9.Septiono W, Kuipers M, Ng N, Kunst A. (2019) Progress of smoke-free policy adoption at district level in Indonesia: A policy diffusion study. Int J Drug Policy. 71, 93-102.
- 10.Chen J, McGhee S, Lam T. (2017) Economic Costs Attributable to Smoking in Hong Kong in 2011: A Possible Increase from 1998. Nicotine Tob Res. DOI: http://dx.doi.org/10.1093/ntr/ntx254 21(4), 505-512.
- 11.Tautolo E, Schluter P, Paterson J, McRobbie H.Acculturation status has a modest effect on smoking prevalence among a cohort of Pacific fathers in New Zealand. , Aust N Z J Public Health 35(6), 509-16.
- 12.Ramsey M, Chen-Sankey J, Reese-Smith J, Choi K. (2019) Association between marital status and cigarette smoking: Variation by race and ethnicity. Prev Med. 119, 48-51.
- 13.Linhart C, Tukana I, Lin S, Taylor R, Morrell S et al. (2017) Declines and plateaux in smoking prevalence over three decades in Fiji. Nicotine Tob Res. 19(11), 1315-1321.
- 14.Chiolero A, Faeh D, Paccaud F, Cornuz J.Consequences of smoking for body weight, body fat distribution, and insulin resistance. , Am J Clin Nutr 87(4), 801-9.
- 15.Duncan M, Freiberg M, Greevy R, Kundu S, Vasan R et al. (2019) Association of Smoking Cessation with Subsequent Risk of Cardiovascular Disease. , JAMA 322(7), 642-650.
- 16.Karimiankakolaki Z, MazloomyMahmoodabad S, Kazemi A, Fallahzadeh H. (2019) Self-efficacy and perceived barriers of pregnant women regarding exposure to second-hand smoke at home. J Educ Health Promot. 29-8.
- 17.Heale R, Griffin M.Self-efficacy with application to adolescent smoking cessation: a concept analysis. , J Adv Nurs 65(4), 912-8.
- 18.Haaga D, Kaufmann A, Malloy E. (2020) Looming Vulnerability and Smoking Cessation Attempts. Nicotine Tob Res. 22(9), 1439-1445.
- 19.Martinez E, K L Tatum, Glass M, Bernath A, Ferris D et al.Correlates of smoking cessation self-efficacy in a community sample of smokers. , Addict Behav 35(2), 175-8.
- 20.Rollins E, Terrion J.Explorations of Self-Efficacy: Personal Narratives as Qualitative Data in the Analysis of Smoking Cessation Efforts. , J. Smok. Cessat 5(1), 57-68.
- 21.Hiscock R, Judge K, Bauld L.Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation?. , J Public Health (Oxf) 33(1), 39-47.
- 22.Lee C, Kahende J. (2000) Factors Associated With Successful Smoking Cessation in the United States. , Am J Public Health 97(8), 1503-1509.
- 23.Georgiadou C, Lavdaniti M, Psychogiou M, Tzenalis A, Sgantzos M et al.Factors affecting the decision to quit smoking of the participants of a hospital-based smoking cessation program in Greece. , J Caring Sci 4(1), 1-11.
- 24.Baheiraei A, Hamzehgardeshi Z, Mohammadi M, Nedjat S, Mohammadi E.Personal and Family Factors Affecting Life Time Cigarette Smoking Among Adolescents in Tehran (Iran): A Community Based Study. , Oman Med J 28(3), 184-90.
- 25.Yasar Z, Kurt Kar, Talay O, F, Kargi A. (2014) One-Year Follow-up Results of Smoking Cessation Outpatient Clinic: Factors Affecting the Cessation of Smoking. Eurasian. 16(2), 99-104.
- 26.Dino G, Kamal K, Horn K, Kalsekar I, Fernandes A. (2004) Stage of change and smoking cessation outcomes among adolescents. Addictive Behaviors. 29(5), 935-940.
- 27.W F Velicer, C, J S Rossi, J O Prochaska.Relapse situations and self-efficacy: An integrative model. , Addict Behav 15(3), 271-83.
- 28.Gallus S, Muttarak R, Franchi M, Pacifici R, Colombo P et al.Why do smokers quit?. , Eur J Cancer Prev 22(1), 96-101.
- 29.Komiyama M, Takahashi Y, Tateno H, Mori M, Nagayoshi N et al. (2019) Support for Patients Who Have Difficulty Quitting Smoking: A Review. Intern Med. 58(3), 317-320.
- 30.Wells M, Aitchison P, Harris F, Ozakinci G, Radley A et al.Barriers and facilitators to smoking cessation in a cancer context: A qualitative study of patient, family and professional views. , BMC Cancer 17(1), 348-10.
- 31.Li I, Lee S, Chen C, Jeng Y, Chen Y.Facilitators and Barriers to Effective Smoking Cessation: Counselling Services for Inpatients from Nurse-Counsellors’ Perspectives — A Qualitative Study. , Int J Environ Res Public Health 11(5), 4782-98.
- 32.C van Rossem, Spigt M, Kleijsen J, Hendricx M, C van Schayck et al.Smoking cessation in primary care: Exploration of barriers and solutions in current daily practice from the perspective of smokers and healthcare professionals. , Eur J Gen Pract 21(2), 111-7.
- 33.Harakeh Z, Scholte R, Vermulst A, Vries H. (2004) Parental factors and adolescents' smoking behavior: an extension of the theory of planned behavior. Preven Med. 39(5), 951-961.
- 34.Takagi D, Kondo N, Takada M, Hashimoto H.Differences in spousal influence on smoking cessation by gender and education among Japanese couples. , BMC Public Health 2014, 1184-10.
- 35.J N Soulakova, C Y Tang, S A Leonardo, L A Taliaferro. (2018) Motivational Benefits of Social Support and Behavioural Interventions for Smoking Cessation. J Smok Cessat. 13(4), 216-226.
- 36.Jiang Y, Elton-Marshall T, Fong G, Li Q. (2010) Quitting smoking in China: findings from the ITC China Survey. Tob Control. 19, 12-17.
- 37.Pisinger C, Aadahl M, Toft U, Jørgensen T.Motives to quit smoking and reasons to relapse differ by socioeconomic status. , Prev Med 2011, 48-52.
- 38.Bonevski B, Regan T, Paul C, Baker A, Bisquera A.Associations between alcohol, smoking, socioeconomic status and comorbidities: Evidence from the 45 and Up Study. Drug Alcohol Rev. 33(2), 169-76.
- 39.Paul C, Ross S, Bryant J, Hill W, Bonevski B et al.The social context of smoking: A qualitative study comparing smokers of high versus low socioeconomic position. , BMC Public Health 2010, 211-10.
- 40.Hiscock R, Bauld L, Amos A, Fidler J, Munafò M.Socioeconomic Status And Smoking: A Review. , Ann N Y Acad Sci 2012, 107-23.
- 41.Abdulghani H.Alrowais, Alhaqwi, Alrasheedi, Al- Zaher, Al-Madani, Al-Eissa, Al-Hakmi, Takroni and Ahmad. Cigarette smoking among female students in five medical and nonmedical colleges. , Int J Gen Med 2013, 719-727.
- 42.Carter-Pokras O, Feldman R, Kanamori M, Rivera I, Chen L et al.Barriers and Facilitators to Smoking Cessation Among Latino Adults. , J Natl Med Assoc 103(5), 423-31.
- 43.Villanti A, BoverManderski M, Gundersen D, Steinberg M, Delnevo C. (2016) Reasons to quit and barriers to quitting smoking in US young adults. Fam Pract. 33(2), 133-139.
- 44.Chad J Gwaltney, Metrik Jane, Christopher W Kahler, Shiffman Saul. (2009) Self-Efficacy and Smoking Cessation: A Meta-Analysis. Psychol Addict Behav. 23(1), 10-1037.
- 45.Chean K, Goh L, Liew K, Tan C, Choi X et al.Barriers to smoking cessation: a qualitative study from the perspective of primary care. in Malaysia. BMJ Open. 2019; 9(7): e025491 10-1136.
- 46.Sagayadevan V, Abdin E, Shahwan S, Satghare P, Devi F et al.Motivations to quit smoking and challenges faced during cessation among individuals with first episode psychosis in Singapore. Early Interv Psychiatry. 13(6), 1488-1494.
- 47.J O Prochaska.Strong and Weak Principles for Progressing from Precontemplation to Action Based on Twelve Problems Behavior. Health Psychol. 13(1), 47-51.
- 48.Milcarz K, Polańska K, Balwicki Ł, Makowiec-Dąbrowska T, Hanke W et al.Perceived barriers and motivators to smoking cessation among socially-disadvantaged populations in Poland. , Int J Occup Med Environ Health 32(3), 363-377.
